Impact des consommations et abus d`alcool chez les

© L’Encéphale, Paris, 2008. Tous droits réservés.
L’Encéphale (2007) Supplément 5, S192-S196
journal homepage : www.elsevier.com/locate/encep
La prévalence d’un mésusage d’alcool actuel chez les
patients hospitalisés se situe entre 12 et 60 % et pour la vie
entière entre 48 et 64 % [5, 8, 9, 25, 32].
Pour les patients en ambulatoire cette prévalence varie
entre 6 et 60 % [21, 28]. L’étendue de la fourchette des
prévalences pose certaines questions notamment sur les
instruments de défi nition et de diagnostic de l’abus/dépen-
dance à l’alcool, et sur les populations évaluées dans ces
études.
D’autres données épidémiologiques sont intéressantes,
concernant les patients présentant un premier épisode psy-
chotique pour lesquels le taux d’abus ou de dépendance est
estimé entre 23 et 37 %. Dans une revue de la littérature,
Drake et Mueser [18] ont trouvé une prévalence sur la vie
entière de 50 % et sur les 6 derniers mois de 25 à 30 %.
Dans le classement des substances toxicomanogènes les
plus utilisées par le patient schizophrène, l’alcool vient au
deuxième rang (45 à 60 % des patients, [23]) après la nico-
tine (70 % des patients dépendants [45]).
En troisième rang vient le cannabis pour 31 à 42 % aux
États-Unis [17], 27 % en France [14], 18,7 % dans le Royaume-
Uni [20] et entre 5 et 13 % en Allemagne [24, 41].
Ces phénomènes d’abus/dépendance subissent des
variations en fonction du temps : en effet la prévalence des
addictions chez les patients souffrant de schizophrénie
augmente depuis les années 60 avec les changements des
modèles de consommation. Ainsi en 1983, aux États-Unis,
la consommation de cannabis était supérieure à celle de la
Impact des consommations et abus d’alcool
chez les sujets psychotiques
R. Schwan(a), L. Malet(b)
(a) CHU de Nancy, Service de Psychiatrie
(b) CHU de Clermont-Ferrand, Service de Psychiatrie
Introduction
Les critères de classifi cation psychiatriques appartiennent à
deux modèles psychopathologiques distincts : le modèle
syndromique et le modèle étiopathogénique. Affi rmer la
coexistence d’un abus ou d’une dépendance à l’alcool et
d’une autre pathologie psychiatrique peut être assez déli-
cat. Dans une approche syndromique, divers symptômes
peuvent être communs aux différents troubles et, un double
diagnostic n’est souvent retenu que pour les formes les plus
sévères. Les études épidémiologiques montrent toutefois
une forte prévalence de l’association comorbide des trou-
bles addictifs et des troubles psychotiques. Inévitablement,
la forte association de deux troubles conduit à s’interroger
sur l’étiopathogénie avec l’enjeu thérapeutique que cela
suppose.
D’après l’étude ECA [39] menée sur 20 000 sujets en
population générale, la schizophrénie est la 2e comorbidité
avec l’addiction (après la personnalité antisociale). Le taux
d’abus ou de dépendance aux substances psychoactives au
cours de la vie chez les patients souffrant de schizophrénie
est de 47 % dont 27,5 % pour les toxicomanies autres que
l’alcool. Le risque relatif d’abus/dépendance pour le sujet
schizophrène sur la vie entière est estimé à 4,6.
Ces données ont été confi rmées par l’étude NCS [26],
réalisée en 1991 sur 8 000 personnes qui rapporte un taux
de comorbidité au cours de la vie de 44,8 % entre psychose
et abus/dépendance aux drogues illicites.
* Auteur correspondant.
E-mail : r.schwan@chu-nancy.fr
L’auteur n’a pas signalé de confl its d’intérêts.
4509_17_Schwan. i ndd 1924509_17_Schwan.indd 192 14/ 12/ 07 14: 59: 2914/12/07 14:59:29
> XPress 6 Noir

Impact des consommations et abus d’alcool chez les sujets psychotiques S193
cocaïne. Cette tendance s’est inversée à partir des années
1990. Ces variations concordent avec les évolutions des
modèles d’abus dans la population générale américaine.
Le type de toxique varie aussi en fonction du pays : en
France l’alcool et le cannabis sont les substances les plus
consommées. Les psycho-stimulants et la cocaïne sont
notablement plus utilisés aux USA. De même pour la
consommation d’hallucinogènes plus marquée aux USA et
faible en Europe. En France, la consommation d’opiacés
est plus marquée mais aussi celle du tabac et du café.
En conclusion du volet épidémiologique, les patients
présentant un double diagnostic ne représentent plus un
groupe marginal dans la population des patients soignés en
psychiatrie mais un groupe central.
Excès de comorbidité
L’épidémiologie descriptive permet de mettre en évidence
la fréquence d’un trouble et de l’association de différents
troubles dans des populations déterminées. Lorsque la pré-
valence de ce trouble en population générale des questions
étiopathologiques, évolutives, diagnostiques et de prise en
charge se posent.
Hypothèses concernant les surmorbidités
Nombre de schizophrènes rapportent l’usage de substances
aussi bien pour éviter l’ennui que pour soulager des symp-
tômes anxieux ou dépressifs, pour réduire les effets des
traitements prescrits ou encore contrebalancer les symptô-
mes négatifs de la schizophrénie [33]. Plusieurs hypothèses
sont formulées pour expliquer la fréquente association
comorbide entre schizophrénie et abus de substances.
1. L’hypothèse symptomatologique qui veut que l’ad-
diction soit un symptôme du trouble psychotique : ce symp-
tôme devrait alors varier comme un marqueur d’état.
2. L’hypothèse du développement secondaire de l’addic-
tion chez des patients présentant un trouble psychotique
a. L’automédication : L’abus/dépendance se situe alors
après l’émergence du trouble ou avant et masquerait les
formes subsyndromiques prodromales.
b. Régulation de l’affect
c. Modèle de super sensitivité : modèle de vulnérabilité
au stress que serait l’alcool.
d. L’hypothèse du glissement social.
3. L’hypothèse de l’induction du trouble psychotique
causée par la consommation d’alcool.
4. L’hypothèse d’une étiologie commune
a. Des facteurs de risque (génétiques) communs
b. Dysfonctionnement neurobiologique primaire dans le
système central dopaminergique (tempête dopaminergi-
que).
c. Trouble de la personnalité.
Aspects évolutifs
L’aspect le plus frappant en clinique chez les patients pré-
sentant une comorbidité schizophrénie-dépendance à l’al-
cool est le phénomène de la porte tournante qui se traduit
par une augmentation considérable du nombre de rechutes
et d’hospitalisations dans cette population.
Chez les patients schizophrènes présentant un compor-
tement violent, on retrouve une prévalence d’abus de
substance de 55,2 % [2]. L’abus de substances multiplie par
4 le risque de violence sur une période de 12 mois [43].
En comparant des schizophrènes présentant un abus/
dépendance à l’alcool à d’autres patients souffrant d’autres
pathologies psychiatriques, Angermeyer, [4] objective une
augmentation de l’OR de 3,9 – 8 concernant le comporte-
ment violent. Le diagnostic associé « d’alcoolisme » aug-
mente l’OR des meurtres chez les hommes de 2,4 et chez
les femmes de 15,9 [22].
La baisse de la compliance au traitement est également
un élément évolutif fréquent [29, 37].
Ces patients comorbides sont plus souvent hospitalisés
aux urgences [11] et leur situation sociale est nettement
plus diffi cile avec un nombre plus important de sujets sans
domicile fi xe.
Au niveau clinique, la symptomatologie est plus intense
avec davantage d’hallucinations [38], de symptômes de
paranoïa [19], des symptômes délirants, plus souvent chro-
niques [5], de symptômes dépressifs [38], une augmenta-
tion du score PANSS [28] et une augmentation du nombre
des tentatives de suicide [35].
Les fonctions cognitives sont également altérées notam-
ment la mémoire, le verbal learning avec une diminution
de la capacité de rétention des mots mais on ne signale pas
de différences concernant la proportion des mots retenus
après un délai et pas de différence concernant le bénéfi ce
après des apprentissages répétés [31]. Il existe aussi une
altération des facteurs cognitifs – perceptuels mesurés par
la Neurologic Evaluation Scale [3].
Manning et al. en comparant des sujets schizophrènes à
des sujets ayant une comorbidité schizophrénie avec abus/
dépendance à l’alcool trouvent qu’il n’existe pas une addi-
tion des effets des deux pathologies mais que fi nalement
les performances cognitives sont assez proches sur certains
points [27].
Impact sur la morphologie cérébrale
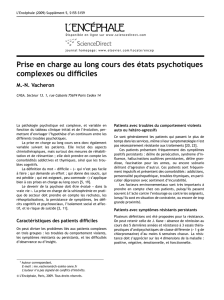
Sullivan et al. ont mené une étude d’imagerie sur l’impact de
l’alcool sur les structures cérébrales en comparant des
patients alcooliques, des schizophrènes sans comorbidités,
des schizophrènes dépendants à l’alcool selon le type de trai-
tement qu’ils reçoivent : neuroleptique typique ou atypique.
Les patients présentant un double diagnostic ont une
modifi cation du volume des structures pontiques qu’on ne
retrouve pas chez les patients non alcooliques. Ces modifi -
cations touchent aussi d’autres régions cérébrales notam-
ment le thalamus et remettent en question les résultats
d’études précédentes sur la schizophrénie qui ne prenaient
pas en compte l’intoxication alcoolique et imputaient les
anomalies à la schizophrénie [42].
D’autres études, ont exploré l’effet de l’alcool sur les
structures cérébrales à distance du sevrage alcoolique et
ont retrouvé des résultats intéressants notamment l’effet
4509_17_Schwan. i ndd 1934509_17_Schwan.indd 193 14/ 12/ 07 14: 59: 3214/12/07 14:59:32
> XPress 6 Noir

R. Schwan, L. MaletS194
nocif de la consommation d’alcool sur le noyau accumbens
chez les patients schizophrènes, partiellement réversible
avec l’abstinence [15] (Fig. 1).
D’autres études ne retrouvent pas de différence volu-
métrique des structures cérébelleuses entre patients schi-
zophrènes et patients alcoolo-dépendants [46].
Nesvag et al. concluent que l’alcool est un facteur
important dans la variation de la morphologie cérébrale
chez les patients schizophrènes [34].
Diagnostic de la comorbidité schizophrénie
– abus/dépendance à l’alcool
Le diagnostic d’un mésusage d’alcool chez les patients pré-
sentant une schizophrénie est complexe. En effet, les
symptômes les plus ostentatoires d’une dépendance à l’al-
cool (le syndrome de sevrage et la tolérance) sont souvent
atténués voire masqués par la prescription des benzodiazé-
pines. Il existe de nombreux outils de dépistage d’un mésu-
sage d’alcool (biologiques, psychométriques, etc.). Mais
alors que ceux-ci sont très bien évalués en population géné-
rale, il n’existe que peu d’études qui se soient intéressées
à l’évaluation de ces outils chez les patients présentant un
double diagnostic. De plus, ces travaux restent souvent
limités et imprécis quant à la description de la population
des patients présentant une schizophrénie (pas d’évalua-
tion psychométrique etc.) ou au type de mésusage d’alcool
(usage nocif, dépendance) (Tableau 1).
L’emploi de ces instruments pose néanmoins quelques
problèmes notamment la période à laquelle ils sont admi-
nistrés qui peut faire varier les résultats.
Malheureusement, de nombreuses études utilisent encore
les critères du DSM IV, ce qui limite considérablement leur
apport ces critères n’étant pas les plus pertinents.
Prise en charge
Plusieurs modalités de prise en charge sont envisageables.
Des traitements psychiatriques et addictologiques consécu-
tifs sont assez fréquents. Pour le psychiatre, l’alcoolisme
peut être vu comme un marqueur d’état qui s’améliorera si
la symptomatologie psychotique du patient s’améliore.
L’addictologue pourra préférer traiter d’abord le mésusage
du produit avant d’envisager un relais en psychiatrie si le
trouble psychiatrique persiste. Une prise en charge séquen-
tielle dépendra en fait essentiellement de la présentation
clinique initiale et des modalités d’accès aux soins. Les
soins psychiatriques et addictologiques peuvent être simul-
tanés, soit en parallèle c’est-à-dire de façon indépendante,
soit de façon partagée avec une étroite collaboration et
une bonne communication entre les équipes. Les interven-
tions de chacun doivent alors être soigneusement plani-
fi ées.
Les approches intégrées, pour lesquelles le même clini-
cien (ou la même équipe) prend en charge aussi bien le
trouble psychiatrique que l’addiction, semblent les plus
effi caces (Fig. 2).
Figure 1 Variations de volume de structures cérébrales
selon les catégories diagnostiques.
–2
–1.5
–1
–0.5
0
0.5
Caudate Putamen NA
All alcoholics, with and without
comorbid Schizophrenia
Volumes (Z-score)
Recently sober
(< 3 weeks) Longer sober
(>3 weeks)
–2
–2.5
–1.5
–1
–0.5
0
0.5
Caudate Putamen NA
Volumes (Z-score)
Alcoholic:
recently sober
Comorbid:
recently sober
Alcoholic:
longer sober
Comorbid:
longer sober
Tableau 1 Outils de dépistage d’un mésusage d’alcool utilisés chez des patients présentant un double diagnostic
Auteur n Test Golden standard Résultats
Dervaux et al. [13] 114 CAGE DSM-III-R Sensitivité 0,82
Spécifi cité : 0,94
Dawe et al. [12] 71 AUDIT SDI, CIDI Sens : 0,87
Spec : 0,90
McHugo et al. [30] 75 MAST Dossier patient Sens : 0,85
Spec : 0,80
Searles et al. [39] 29 MAST DSM-III
Toland et al. [43] 20 GGT, MCV, ASAT, ALAT, MAST Entretien clinique
Agelink et al. [1] 70 GGT, CDT Sens CDT : 58,8 %
Sens GGT : 70,6
4509_17_Schwan. i ndd 1944509_17_Schwan.indd 194 14/ 12/ 07 14: 59: 3314/12/07 14:59:33
> XPress 6 Noir

Impact des consommations et abus d’alcool chez les sujets psychotiques S195
Des études ont été menées pour évaluer l’effi cacité de
ces programmes. Bartels et al trouvent des taux de rémis-
sion de l’ordre de 44 % pour l’abus d’alcool et de 41 % pour
les drogues chez 148 patients suivis pendant 7 ans [7].
Detrick et Stiepock rapportent un taux de sortie d’étude
de 0 % lors du suivi sur 18 mois de 17 patients [16].
De Leon et al., 2000 trouvent un taux de sortie des pro-
grammes moindre lorsqu’il s’agit de programmes intégrés
(étude sur 342 patients sans domicile fi xe).
Barrowclough observe moins de symptômes psychoti-
ques dans le groupe programme intégré sur une population
de 18 patients randomisés et suivis pendant 21 mois [6].
Références
[1] Agelink MW, Ullrich H, Lemmer W et al. Screening for con-
comitant alcohol abuse in schizophrenia : clinical significance
of the Munich Alcoholism Test and laboratory tests. Eur Addict
Res 1999 ; 5 : 82-7.
[2] Allebeck P. Schizophrenia : a life-shortening disease. Schizo-
phr Bull 1989 ; 15 : 81-9.
[3] Allen DN, Goldstein G, Forman SD et al. Neurologic examina-
tion abnormalities in schizophrenia with and without a history
of alcoholism. Neuropsychiatry Neuropsychol Behav Neurol
2000 ; 13 : 184-7.
[4] Angermeyer MC. Schizophrenia and violence. Acta Psychiatr
Scand Suppl 2000 ; 63-7.
[5] Barbee JG, Clark PD, Crapanzano MS et al. Alcohol and sub-
stance abuse among schizophrenic patients presenting to an
emergency psychiatric service. J Nerv Ment Dis 1989 ; 177 :
400-7.
[6] Barrowclough C, Haddock G, Tarrier N et al. Randomized con-
trolled trial of motivational interviewing, cognitive behavior
therapy, and family intervention for patients with comorbid
schizophrenia and substance use disorders. Am J Psychiatry
2001 ; 158 ; 1706-13.
[7] Bartels SJ, Drake RE, Wallach MA. Long-term course of sub-
stance use disorders among patients with severe mental ill-
ness. Psychiatr Serv 1995 ; 46 : 248-51.
[8] Brady K, Casto S, Lydiard RB et al. Substance abuse in an
inpatient psychiatric sample. Am J Drug Alcohol Abuse 1991 ;
17 : 389-97.
[9] Cantwell R, Brewin J, Glazebrook C et al. Prevalence of sub-
stance misuse in first-episode psychosis. Br J Psychiatry 1999 ;
174 : 150-3.
[10] Comtois KA, Russo JE, Roy-Byrne P et al. Clinicians’ assess-
ments of bipolar disorder and substance abuse as predictors
of suicidal behavior in acutely hospitalized psychiatric inpa-
tients. Biol Psychiatry 2004 ; 56 : 757-63.
[11] Craig TJ, Lin SP, El-Defrawi MH et al. Clinical correlates of
readmission in a schizophrenic cohort. Psychiatr Q 1985 ; 57 :
5-10.
[12] Dawe S, Seinen A, Kavanagh D. An examination of the utility
of the AUDIT in people with schizophrenia. J Stud Alcohol
2000 ; 61 : 744-50.
[13] Dervaux A, Bayle FJ, Laqueille X et al. Validity of the CAGE
questionnaire in schizophrenic patients with alcohol abuse
and dependence. Schizophr Res 2006 ; 81 : 151-5.
[14] Dervaux A, Laqueille X, Bourdel MC et al. Cannabis and schiz-
ophrenia : demographic and clinical correlates. Encéphale
2003 ; 29 : 11-17.
[15] Deshmukh A, Rosenbloom MJ, De Rosa E et al. Regional stri-
atal volume abnormalities in schizophrenia : effects of comor-
bidity for alcoholism, recency of alcoholic drinking, and
antipsychotic medication type. Schizophr Res 2005 ; 79 : 189-
200.
[16] Detrick A, Stiepock V. Treating persons with mental illness,
substance abuse, and legal problems : the Rhode Island expe-
rience. New Dir Ment Health Serv 1992 ; 65-77.
[17] Dixon L, Haas G, Weiden PJ et al. Drug abuse in schizophrenic
patients : clinical correlates and reasons for use. Am J Psy-
chiatry 1991 ; 148, 224-30.
[18] Drake RE, Mueser KT. Psychosocial approaches to dual diagno-
sis. Schizophr Bull 2000 ; 26 : 105-18.
[19] Drake RE, Wallach MA, Teague GB et al. Housing instability
and homelessness among rural schizophrenic patients. Am J
Psychiatry 1991 ; 148 : 330-6.
[20] Duke PJ, Pantelis C, McPhillips MA et al. Comorbid non-alco-
hol substance misuse among people with schizophrenia : epi-
demiological study in central London. Br J Psychiatry 2001 ;
179 : 509-13.
[20] El-Guebaly N, Hodgins DC. Schizophrenia and substance
abuse : prevalence issues. Can J Psychiatry 1992 ; 37 : 704-
10.
[22] Eronen M, Hakola P, Tiihonen J. Mental disorders and homi-
cidal behavior in Finland. Arch Gen Psychiatry 1996 ; 53 : 497-
501.
[23] Hambrecht M, Hafner H. Substance abuse and the onset of
schizophrenia. Biol Psychiatry 1996 ; 40 : 1155-63.
[24] Hambrecht M, Hafner H. Cannabis, vulnerability, and the
onset of schizophrenia : an epidemiological perspective. Aust
N Z J Psychiatry 2000 ; 34 : 468-75.
[25] Havassy BE, Arns PG. Relationship of cocaine and other sub-
stance dependence to well-being of high-risk psychiatric
patients. Psychiatr Serv 1998 ; 49 : 935-40.
[26] Kendler KS, Gallagher TJ, Abelson JM et al. Lifetime preva-
lence, demographic risk factors, and diagnostic validity of
nonaffective psychosis as assessed in a US community sample.
The National Comorbidity Survey. Arch Gen Psychiatry 1996 ;
53 : 1022-31.
[27] Manning V, Wanigaratne S, Best D et al. Screening for cogni-
tive functioning in psychiatric outpatients with schizophre-
nia, alcohol dependence, and dual diagnosis. Schizophr Res
2007 ; 91 : 151-8.
[28] Margolese HC, Malchy L, Negrete JC et al. Drug and alcohol
use among patients with schizophrenia and related psycho-
ses : levels and consequences. Schizophr Res 2004 ; 67 : 157-
66.
Figure 2 Programme de prise en charge spécifi que d’un
trouble comorbide d’après Gouzoulis-Mayfrank, 2004.
Facteurs
neurobiologiques
communs (tempête
dopaminergique)
Trait de personnalité
communs (cluster
d’une PAS, impulsivité,
coping avec du stress)
Environnement
social
Motivation
individuelle
à consommer
Effets secondaires
du traitement
antidopaminergique
Schizophrénie
Mésusage
Super sensitivité
pour les substances
1° symptômes
de la psychose
Sypmtômes
dépressifs
Symptômes positifs
Symptômes négatifs
4509_17_Schwan. i ndd 1954509_17_Schwan.indd 195 14/ 12/ 07 14: 59: 3314/12/07 14:59:33
> XPress 6 Noir

R. Schwan, L. MaletS196
[29] McFarland BH, Faulkner LR, Bloom JD et al. Chronic mental
illness and the criminal justice system. Hosp Community Psy-
chiatry 1989 ; 40 : 718-23.
[30] McHugo GJ, Paskus TS, Drake RE. Detection of alcoholism in
schizophrenia using the MAST. Alcohol Clin Exp Res 1993 ; 17 :
187-91.
[31] Mohamed S, Bondi MW, Kasckow JW et al. Neurocognitive
functioning in dually diagnosed middle aged and elderly
patients with alcoholism and schizophrenia. Int J Geriatr Psy-
chiatry 2006 ; 21 : 711-8.
[32] Mueser KT, Levine S, Bellack AS et al. Social skills training for
acute psychiatric inpatients. Hosp Community Psychiatry
1990 ; 41 : 1249-51.
[33] Mueser KT, Nishith P, Tracy JI et al. Expectation and motives
for substance use in schizophrenia. Psychiatric Clinics of
North America 1995 ; 21 (3) : 367-78.
[34] Nesvag R, Frigessi A, Jonsson EG et al. Effects of alcohol con-
sumption and antipsychotic medication on brain morphology
in schizophrenia. Schizophr Res 2007 ; 90 : 52-61.
[35] Nixon SJ, Hallford HG, Tivis RD. Neurocognitive function in
alcoholic, schizophrenic, and dually diagnosed patients. Psy-
chiatry Res 1996 ; 64 : 35-45.
[36] Noreik K. Attempted suicide and suicide in functional psycho-
ses. Acta Psychiatr Scand 1975 ; 52 : 81-106.
[37] Pristach CA, Smith CM. Medication compliance and substance
abuse among schizophrenic patients. Hosp Community Psy-
chiatry 1990 ; 41 : 1345-8.
[38] Pulver AE, Wolyniec PS, Wagner MG et al. An epidemiologic
investigation of alcohol-dependent schizophrenics. Acta Psy-
chiatr Scand 1989 ; 79 : 603-12.
[39] Regier DA, Farmer ME, Rae DS et al. Comorbidity of mental
disorders with alcohol and other drug abuse. Results from the
Epidemiologic Catchment Area (ECA) Study. Jama 1990 ; 264 :
2511-8.
[40] Searles JS, Alterman AI, Purtill JJ. The detection of alcohol-
ism in hospitalized schizophrenics : a comparison of the MAST
and the MAC. Alcohol Clin Exp Res 1990 ; 14 : 557-60.
[41] Soyka M, Albus M, Kathmann N et al. Prevalence of alcohol
and drug abuse in schizophrenic inpatients. Eur Arch Psychia-
try Clin Neurosci 1993 ; 242 : 362-72.
[42] Sullivan EV, Rosenbloom MJ, Serventi KL et al. Effects of alco-
hol dependence comorbidity and antipsychotic medication on
volumes of the thalamus and pons in schizophrenia. Am J Psy-
chiatry 2003 ; 160 : 1110-6.
[43] Swanson JW, Holzer CE, 3rd Ganju VK et al. Violence and psy-
chiatric disorder in the community : evidence from the Epide-
miologic Catchment Area surveys. Hosp Community Psychiatry
1990 ; 41 : 761-70.
[44] Toland AM, Moss HB. Identification of the alcoholic schizo-
phrenic : use of clinical laboratory tests and the MAST. J Stud
Alcohol 1989 ; 50 : 49-53.
[45] Van Dongen CJ. Smoking and persistent mental illness : an
exploratory study. J Psychosoc Nurs Ment Health Serv 1999 ;
37 : 26-34.
[46] Varnas K, Okugawa G, Hammarberg A et al. Cerebellar vol-
umes in men with schizophrenia and alcohol dependence.
Psychiatry Clin Neurosci 2007 ; 61 : 326-9.
4509_17_Schwan. i ndd 1964509_17_Schwan.indd 196 14/ 12/ 07 14: 59: 3314/12/07 14:59:33
> XPress 6 Noir
1
/
5
100%