Cardiomyopathie du péripartum - Département d`Anesthésie du

Cardiomyopathie du péripartum
Staff d’Anesthésie du Lundi 20 Avril
2015
CHI Poissy St-Germain
Sarah Féray – Interne
!

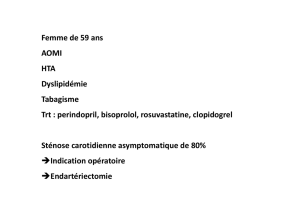
Cas clinique
Madame TK, 36 ans, origine africaine
• Antécédents médicaux :
– Obésité IMC = 33
– Aucun FdR cardiovasculaire
• Antécédents obstétricaux :
– G3P3 :
– AVB en 2007 (4250g)
– AVB en 2009 (4950g)
– AVB en 2011 (5120g)
• Antécédents chirurgicaux : aucun
• Allergie : non connue
!

Histoire de la maladie
• Hospitalisé à 10 mois de sa dernière grossesse pour
décompensation cardiaque globale
• Se plaint depuis 2 mois d’une dyspnée d’effort
Examen clinique initial :
• Etat général conservé, apyrétique, TA 120/70, FC 90/min
• Dyspnée NYHA III
• Bruit du Coeur régulier, souffle systolique de 3/6ème mitral
• Signes d’insuffisance cardiaque gauche : crépitants aux
bases pulmonaires
• Signes d’insuffisance cardiaque droite : OMI,
hepatomegalie, reflux hépato-jugulaire

Examens complémentaires
• ECG : ryhtme sinusal à 90/min, trouble de la repolarisation non
spécifique
• Radio thorax : cardiomégalie, syndrome interstitiel accentué au
hile
• Biologie : normale sauf NTproBNP 2000 pg/ml, troponine
négative
• ETT :
VG dilaté - parois normotrophiques avec hypokinésie globale
FEVG = 33%
OG dilatée
Cavités droites non dilatés, pas d’HTAP
Fuite mitrale modérée

Diagnostic et PEC
• Insuffisance cardiaque globale sur cardiomyopathie
dilatée, hypokinétique, non connue auparavant chez une
patiente de 36 ans
• Hypothèse : cardiomyopathie dilatée liée à la grossesse
! Coroscanner : normal
! IRM cardiaque : cardiomyopathie dilatée non ischémique,
VG dilaté, FE à 33%.
Pas d’étiologie spécifique retrouvée = élimination diagnostic
différentiel
• Traitement médical débuté : Triatec, Bisoprolol, Lasilix,
Kardégic
!
 6
6
 7
7
 8
8
 9
9
 10
10
 11
11
 12
12
 13
13
 14
14
 15
15
 16
16
 17
17
 18
18
 19
19
 20
20
 21
21
 22
22
 23
23
 24
24
 25
25
 26
26
 27
27
 28
28
 29
29
 30
30
 31
31
 32
32
 33
33
 34
34
 35
35
 36
36
 37
37
 38
38
 39
39
 40
40
1
/
40
100%