Lire l'article complet

Dossier
tmiqu
Le Courrier de la Transplantation - Volume VI - n
o 4 - octobre-novembre-décembre 2006
215
Utilisation de
l’érythropoïétine
recombinante en
transplantation
d’organe
Le traitement de l’anémie
après transplantation hépatique
Y. Calmus*●
U
tilisant comme définition de
l’anémie un taux d’hémoglo-
bine inférieur à 13 g/dl chez
l’homme et à 12 g/dl chez la femme
(American Society of Transplantation),
il a été constaté que la fréquence de
l’anémie après transplantation rénale
était de l’ordre de 20 à 25 % à un an,
dans l’observatoire espagnol MOST (1),
comme dans la série de Toulouse (2). En
revanche, la fréquence de l’anémie est
un problème mal évalué après transplan-
tation hépatique (TH). Les chiffres vont
de 3 % à plus de 50 % (3-6), en fonction
des dénitions utilisées, souvent arbi-
traires, et des traitements immunosup-
presseurs reçus.
Il est intéressant de s’appuyer sur l’ex-
périence en transplantation rénale pour
tenter de dénir les paramètres les plus
fréquemment associés à la présence
d’une anémie : il s’agit en particulier
de la fonction rénale (taux de ltration
glomérulaire), de l’albuminémie, des
marqueurs d’inammation et de l’uti-
lisation de certains médicaments, en
particulier du mycophénolate mofétil
(MMF) ou de l’azathioprine (1, 2, 7), et
à présent du sirolimus (8). La fonction
rénale, l’existence d’une inammation,
l’état nutritionnel et l’utilisation de
médicaments myélosuppresseurs sont
donc les paramètres les plus clairement
associés à la présence d’une anémie
dans ce contexte. Après TH, l’étiologie
de l’anémie n’est reconnue que dans
une minorité de cas, allant, dans la litté-
rature, de 16 à 47 % (3, 4, 9). Dans
la présente mise au point, les causes
précoces d’anémie (15 à 30 premiers
jours post-TH), qui sont essentiellement
les saignements per- et postopératoires
précoces, les infections, les syndromes
inflammatoires, les carences et les
déficits nutritionnels pré-greffe, ne
seront pas abordées. Seules les causes
d’anémie plus tardives, au-delà de J30,
seront envisagées : d’abord les causes
connues, qu’il convient de rechercher
selon un schéma classique (tableau I),
puis les anémies d’origine mal établie,
qui posent d’importants problèmes
thérapeutiques. Dans un troisième
temps sera envisagé le cas particulier
de l’anémie au cours du traitement de
la récidive virale C.
* Service de chirurgie, hôpital Cochin, 75014 Paris.
Le traitement de l’anémie après transplantation hépatique
Y. Calmus
L’anémie chez le patient transplanté rénal
G. Choukroun, M. Jauréguy
L’érythropoïétine, ses dérivés érythropoïétiques
et non érythropoïétiques : vers une cytoprotection ubiquitaire ?
F. Martinez, J. Zuber, E. Thervet
●
●
●
Coordinateurs :
G. Choukroun, CHU Amiens
et F. Martinez, hôpital Necker,
Paris

Dossier
tmiqu
Le Courrier de la Transplantation - Volume VI - n
o 4 - octobre-novembre-décembre 2006
216
LES CAUSES CONNUES
L’hémolyse
Une microangiopathie thrombotique (MAT)
est observée dans 3 à 14 % des transplan-
tations rénales sous anticalcineurines (10).
Son diagnostic repose sur des tests classi-
ques (tableau I). Comme dans les autres
causes de MAT, un décit en métallopro-
téase ADAMTS13 a été mis en évidence
dans ce contexte (11). La responsabilité des
anticalcineurines dans ce décit n’est pas
clairement établie : ils pourraient exercer
un effet inhibiteur direct sur la métallo-
protéase, ou induire l’apparition d’auto-
anticorps dirigés contre elle. La réduction
de la dose d’anticalcineurines (10) ou la
conversion complète à une immunosup-
pression sans anticalcineurines, notamment
à base d’inhibiteurs de mTOR (12), est
la réponse thérapeutique habituellement
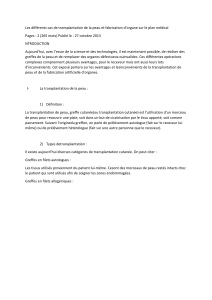
Tableau I. Causes connues d’anémie après transplantation hépatique.
Fréquence après TH Date post-gree Tests diagnostiques Traitement
Hypersplénisme 100 % ? Prédominant en phase précoce.
Constante ensuite ?
Durée de vie des GR,
séquestration splénique
Embolisation
Splénectomie
Virus Parvovirus 19
CMV, EBV
VHB, VHC
1-6 sem. (P19),
1-12 sem. (CMV),
constant (EBV)
PCR,
sérologies,
antigénémie
Antiviraux
IVIg
Décit martial,
décits vitaminiques
10 % chez l’adulte
élevée en cas de perte sanguine
Surtout en phase précoce
Puis : en cas d’ulcères+++
Fer, ferritine, dosage
folates, vitamines B12
Fer, vitamines
Insusance rénale 7-10 % à 7 ans,
18 % à 13 ans pour les formes graves
Augmentant avec le temps Clairance, PBR... EPO
Médicament Fréquent : azathioprine, MMF,
ganciclovir , interféron (myélotoxicité),
ribavirine (hémolyse)
Rare : anticalcineurines (insusance
rénale, anémie hémolytique)
Sirolimus, cotrimoxazole, allopurinol
Corticoïdes, AINS
Constante
Réduction, arrêt
Mesure de fonction rénale,
recherche de saignement
Réduction, conversion,
arrêt
SLP 2-4 % Tardive LDH, bêta-2 microglobulines,
immunoélectrophorèse,
PCR EBV...
Réduction du traitement IS
Traitement du SLP
GVHD 1 % Précoce (2-6 sem.) Recherche de chimérisme Traitement IS
Hémolyse, MAT ? Surtout précoce
Puis toxicité médicamenteuse ?
LDH, haptoglobine,
schizocytes, bilirubine,
test de Coombs
IVIg
Échanges plasmatiques
Changement d’IS
Aplasie < 1 %
5 à 30 % des TH pour HF
d’origine inconnue
Précoce (2-6 sem.) Ponction médullaire Traitement IS
HF : hépatite fulminante ; SLP : syndrome lymphoprolifératif ; LDH : lacticodéshydrogénases ; IS : immunosuppression ; IVIg : immunoglobulines polyvalentes ; AINS : anti-inammatoires non stéroïdiens ;
PBR : ponction-biopsie rénale ; GR : globules rouges ; MAT : microangiopathie thrombotique.

Dossier
tmiqu
Le Courrier de la Transplantation - Volume VI - n
o 4 - octobre-novembre-décembre 2006
217
proposée en cas de MAT. Une prudence
toute particulière doit être apportée lorsque
l’anticalcineurine est simplement réduite,
dans la mesure où l’association inhibiteur
de mTOR et anticalcineurines peut majorer
la MAT (13). Les échanges plasmatiques
et l’administration d’immunoglobulines
polyvalentes sont habituellement proposés
dans les formes graves de MAT.
Les causes virales
L’infection par le Parvovirus 19 est une
cause classique d’anémie après transplan-
tation. Utilisant une technique de PCR
qualitative, l’infection par le Parvovirus
19 a été mise en évidence jusque dans
38 % des cas en cas d’anémie inférieure
à 10 g/dl après transplantation rénale (14).
Dans un autre travail, la présence d’une
PCR positive à deux examens consécutifs
a été constatée chez 12 % des transplantés
rénaux, associée à une anémie (15). Les
traitements antiviraux disponibles sont peu
ou pas efcaces sur le Parvovirus. L’ad-
ministration d’immunoglobulines polyva-
lentes a un effet bénéque (16, 17). Une
réduction du traitement immunosuppres-
seur est une réponse logique, lorsqu’elle
est possible. L’érythropoïétine (EPO) peut
être utile dans les formes résistantes aux
traitements précédents (17).
L’infection par le cytomégalovirus peut
induire une anémie, mais qui est rare-
ment au premier plan ; la leucopénie et
la thrombopénie sont souvent prédomi-
nantes. Le traitement par le ganciclovir
est efcace dans la quasi-totalité des cas.
L’infection par le virus Epstein-Barr peut
induire une anémie, elle aussi rarement au
premier plan. Aucun antiviral disponible
n’est efcace sur ce virus. Le traitement
repose sur la réduction du traitement
immunosuppresseur et sur l’utilisation
des traitements appropriés en cas de
syndrome lymphoprolifératif associé. Les
infections par le virus de l’hépatite B ou
de l’hépatite C ne semblent pas jouer de
rôle important dans l’anémie post-TH.
Les causes médicamenteuses
L’utilisation de MMF ou d’azathio-
prine est clairement associée à un
risque accru d’anémie. Dans le travail
prospectif randomisé de Wiesner et
al., qui comparait l’intérêt respectif du
MMF et de l’azathioprine associés à
la ciclosporine et aux corticoïdes (5),
une anémie a été constatée dans 43 %
des cas dans le premier groupe et 53 %
dans le second. Il existe une corrélation
entre le dosage médicamenteux et l’ap-
parition d’une anémie : le taux résiduel
d’acide mycophénolique était plus élevé
en cas d’anémie qu’en son absence (18).
L’intérêt d’une mini-aire sous la courbe
(ASC) pour réduire l’anémie n’a pas été
établi dans ce contexte.
Le sirolimus est capable d’induire une
anémie dont le mécanisme est encore mal
établi. Dans un travail récent, Thaunat
et al. (8) ont montré que l’utilisation de
sirolimus était associée à une réduction
moyenne de l’hémoglobine de 2,8 g/dl et
à la diminution du fer sérique, ainsi qu’à
une augmentation de la ferritine et des
autres paramètres d’inammation (CRP,
brinogène, interleukine-6 et TNFα).
Cette anémie était améliorée après inter-
ruption du sirolimus. Ce médicament
pourrait donc induire une anémie par le
biais d’un syndrome inammatoire.
Les inhibiteurs de l’enzyme de conver-
sion (1) et les antagonistes du récepteur
de l’angiotensine II (19) ne semblent pas
avoir d’effet signicatif sur le chiffre
d’hémoglobine.
Le tacrolimus a été incriminé dans d’ex-
ceptionnels cas d’hypoplasie médullaire
sans dysplasie (20), qui s’atténue après
conversion à la ciclosporine.
Carences en fer et en vitamines
Après transplantation rénale, une
carence martiale a été constatée dans
13 % des cas à 12 mois (2). Après
TH, la carence martiale semble rela-
tivement rare : 4 cas seulement sur
59 enfants explorés (4). Par ailleurs,
la carence en folates et en vitamine
B12 semble exceptionnelle après TH
(4). Cette absence de carence en fer et
en vitamines est probablement liée à
l’utilisation presque systématique de
fer et de supplémentations vitaminiques
dans la période postopératoire précoce
après TH. La carence martiale peut
être plus fréquente chez l’adulte (de
l’ordre de 10 %) [3], favorisée par les
pertes digestives. La recherche d’une
œsophagite ou d’une maladie ulcéreuse
gastroduodénale doit être systématique
dans ce contexte.
Aplasie médullaire
L’aplasie médullaire est exception-
nelle après TH. Elle a été observée en
particulier en cas de TH pour hépatite
fulminante de cause inconnue (non-A,
non-B, non-C) [21]. La responsabilité
d’un virus inconnu, dont l’infection est
probablement facilitée par le traitement
immunosuppresseur, a été mise en cause.
L’aplasie médullaire apparaît alors dans
les 10 jours suivant la TH. Le traitement
fait habituellement appel aux immuno-
suppresseurs, en particulier aux globu-
lines antithymocytaires (22).
Une érythroblastopénie, liée à l’appa-
rition d’anticorps, a été constatée chez
des patients recevant un traitement par
l’époétine alpha. Le traitement immu-
nosuppresseur exerce habituellement un
effet bénéque sur cette pathologie (23).
L’utilisation ultérieure d’érythropoïétine
reste possible lorsque les anticorps anti-
EPO ont disparu.
Syndrome lymphoprolifératif
Une anémie hémolytique peut être révé-
latrice d’un syndrome lymphoprolifératif
après transplantation (3). Le traitement
repose sur celui du syndrome lympho-
prolifératif.
Insuffisance rénale
L’existence d’une insuffisance rénale
grave est relativement fréquente après
TH. Elle a été mise en évidence dans au
moins 8 % des cas à 7-ans et 18 % des cas
à 13 ans (24, 25). Par ailleurs, une insuf-
sance rénale modérée est probablement
très fréquente après TH, et très vraisem-
blablement largement sous-évaluée. Le
rôle de cette insufsance rénale modérée
dans la survenue d’une anémie est mal
évalué après TH. Le traitement repose sur
l’EPO.

Dossier
tmiqu
Le Courrier de la Transplantation - Volume VI - n
o 4 - octobre-novembre-décembre 2006
218
Maladie du greffon contre l’hôte
Une maladie du greffon contre l’hôte
(GVHD) symptomatique apparaît dans
environ 1 % des cas, deux à six semaines
après TH (26). Dans les formes les plus
apparentes (27), elles se manifestent
sous forme d’une éruption cutanée,
d’une diarrhée, d’une èvre et d’une
pancytopénie ou d’une anémie. Le
diagnostic est établi sur la constatation
d’un macrochimérisme lymphocytaire,
reposant soit sur une technique de PCR,
mettant en évidence chez le receveur le
système HLA du donneur, soit sur la
cytométrie en flux du sang périphé-
rique, utilisant des anticorps dirigés
contre des groupes HLA du donneur.
Le diagnostic peut également être fait
par la biopsie cutanée ou intestinale
mettant en évidence les groupes HLA
du donneur. Dans le travail de Taylor et
al. (27), dans 33 cas potentiels associant
les signes cliniques habituels de GVHD,
celle-ci n’a été en fait démontrée que
dans sept cas, où la PCR du donneur était
positive et où les lymphocytes circulants
provenant du donneur représentaient 7
à 50 % des lymphocytes circulants. Le
pronostic de la GVHD est relativement
péjoratif. Cette maladie peut être atté-
nuée par la majoration du traitement
immunosuppresseur.
Incompatibilité ABO
L’incompatibilité ABO est rarement
réalisée après TH. Dans ce cas, une
anémie hémolytique liée à la présence
d’isohémagglutinines anti-A ou anti-B
peut être observée 7 à 10 jours après TH,
et dure en moyenne un mois (3).
Hypersplénisme
L’hypersplénisme est une complication
fréquente de l’hypertension portale. Il
a été clairement montré que les signes
d’hypersplénisme s’atténuaient après
TH. En particulier, Yanaga et al. (28)
ont montré que la thrombopénie était
en grande partie réversible, cette réver-
sibilité apparaissant dès deux semaines
après la TH. Cependant, l’existence d’un
hypersplénisme résiduel est relativement
mal établie. L’amélioration de l’anémie
après embolisation splénique, chez des
patients bénéciant d’un traitement de la
récidive virale C après TH (29), suggère
fortement que l’hypersplénisme persiste
de façon dénitive après TH.
ANÉMIES DE CAUSE INCONNUE
Lorsque les causes connues d’anémie
ne sont pas trouvées, ce qui paraît être
le cas le plus fréquent après TH (4, 8),
deux étiologies occultes semblent vrai-
semblables.
La première est la présence d’une insuf-
sance rénale méconnue. La fréquence
de l’insufsance rénale sévère est bien
établie après TH. En revanche, peu de
travaux ont réellement évalué le taux
de ltration glomérulaire à distance de
la TH. Les causes d’insufsance rénale
post-TH ne sont pas seulement liées à
l’utilisation des anticalcineurines. La
néphropathie diabétique, la néphroan-
giosclérose hypertensive et la néphrose
osmotique liée à l’utilisation antérieure
de dérivés de l’amidon (30) sont elles
aussi fréquemment retrouvées lorsqu’une
biopsie rénale est pratiquée à distance
de la TH. Une évaluation précise de la
fonction rénale doit être effectuée en cas
d’anémie inexpliquée post-TH.
Une autre cause probable d’anémie est
le défaut de production d’EPO. Dans le
travail de Misra et al., portant sur l’enfant,
aucune cause d’anémie n’a été trouvée
dans 84 % des cas (4). Parmi ces anémies
d’étiologie inconnue, un tiers présentait
une récupération spontanée, alors que
l’anémie persistait dans les deux autres
tiers. Les patients récupérant spontané-
ment avaient un taux d’EPO et une réti-
culocytose plus élevés que les autres.
Dans le même ordre d’idée, parmi les
facteurs prédictifs d’anémie observés à
12 mois après transplantation rénale, le
taux d’EPO à J0 était un élément indé-
pendant (2).
Bien qu’un travail isolé ait suggéré que
la production d’EPO était normale après
TH (6), il a été constaté dans une autre
série (4) que la réponse EPO était inap-
propriée chez les patients ayant bénécié
d’une TH. Dans un travail récent, nous
avons conrmé (31) que la production
d’EPO était réduite chez les patients ayant
bénécié d’une TH, et que le mécanisme
possible était un effet inhibiteur direct
des anticalcineurines, en particulier de la
ciclosporine, sur la production d’EPO.
La conjonction d’une insufsance rénale
occulte et d’un défaut de production
d’EPO induit par les anticalcineu-
rines pourrait être une cause fréquente
d’anémie post-TH. Dans les deux cas,
la seule réponse thérapeutique possible
est l’administration d’EPO.
LE TRAITEMENT DE LA RÉCIDIVE
VIRALE C APRÈS TH
L’hépatite C est la principale étiologie de
TH aux États-Unis, et la deuxième cause
en Europe après la maladie alcoolique du
foie. En France, 15 à 25 % des patients
bénéciant d’une TH sont porteurs du
virus C au moment de la TH. Chez ces
patients, la récidive virale est constante.
La récidive virale C est souvent plus
agressive que la maladie virale C observée
chez les patients non transplantés : une
cirrhose est constatée dans 20 % environ
des cas à 5 ans après TH (32-34). De ce
fait, les patients ayant subi une transplan-
tation hépatique pour maladie virale C
sont fréquemment amenés à bénécier
d’un traitement antiviral.
L’utilisation d’interféron seul est peu
efcace dans ce contexte, et comporte
surtout un risque élevé de rejet grave.
Aujourd’hui, la totalité des patients
bénécient d’un traitement associant
l’interféron pégylé et la ribavirine
(35-37). L’interféron possède un effet
myélotoxique portant sur les trois lignées
myéloïdes, mais surtout sur les lignées
blanche et plaquettaire. La ribavirine
possède un effet hémolytique. La demi-
vie de la ribavirine est de six jours chez
les patients à fonction rénale normale,
mais cette demi-vie augmente considéra-
blement en présence d’une insufsance
rénale (38).

Dossier
tmiqu
Le Courrier de la Transplantation - Volume VI - n
o 4 - octobre-novembre-décembre 2006
219
L’anémie est la cause la plus fréquente
de réduction de dose ou d’interruption du
traitement chez les patients bénéciant
d’un traitement de la récidive virale C
après TH. L’utilisation d’autres médica
-
ments myélotoxiques est déconseillée
dans ce contexte.
En cas d’insuffisance rénale, une
réduction des doses de ribavirine ou un
espacement des doses sont vivement
conseillés lorsque la clairance est infé-
rieure à 20 ml/mn (38, 39). Un dosage
de ribavirine, non effectué en pratique
courante, pourrait être plus largement
utilisé.
L’utilisation d’EPO permet de main-
tenir le traitement antiviral et de
permettre l’éradication virale même
dans les cas où l’anémie aurait habi-
tuellement conduit à l’interruption
du traitement antiviral (40). Dans un
travail prospectif multicentrique, nous
avons montré que l’utilisation de l’EPO
dans 38 % des cas chez des patients
bénéciant d’un traitement antiviral
après TH permettait de maintenir le
traitement antiviral dans la majorité
des cas (93 %), et augmentait le taux
d’éradication virale (réponse virolo-
gique prolongée dans 40 % des cas de
cette série) [37]. L’utilisation d’EPO
pourrait donc être la réponse adaptée à
ce type de patients. Elle s’accompagne
d’une amélioration de la qualité de vie
chez les patients transplantés (41). ■
RéféRences
bibliogRaphiques
1. Fernandez-Fresnedo G, Palomar R, Rodrigo
E et al. Prevalence of anemia in renal transplant
patients: results from MOST, an observational
trial. Transplant Proc 2005;37:3821-2.
2. Turkowski-Duhem A, Kamar N, Cointault O
et al. Predictive factors of anemia within the
rst year postrenal transplant. Transplantation
2005;80:903-9.
3. Maheshwari A, Mishra R, Thuluvath PJ. Post-
liver-transplant anemia: etiology and management.
Liver Transpl 2004;10:165-73.
4. Misra S, Moore TB, Ament ME, Vargas JH,
Busutill RW, McDiarmid SV. Prole of anemia in
children after liver transplantation. Transplanta-
tion 2000;70:1459-63.
5. Wiesner R, Rabkin J, Klintmalm G et al. A
randomized double-blind comparative study of
mycophenolate mofetil and azathioprine in combi-
nation with cyclosporine and corticosteroids in
primary liver transplant recipients. Liver Transpl
2001;7:442-50.
6. Vasilopoulos S, Hally R, Caro J et al. Erythro-
poietin response to post-liver transplantation
anemia. Liver Transpl 2000;6:349-55.
7. Molnar MZ, Novak M, Ambrus C et al. Anemia
in kidney transplanted patients. Clin Transplant
2005; 19:825-33.
8. Ndimbie OK, Frezza E, Jordan JA, Koch W,
van Thiel DH. Parvovirus B19 in anemic liver
transplant recipients. Clin Diagn Lab Immunol
1996;3:756-60.
9. Schwimmer J, Nadasdy TA, Spitalnik PF, Kaplan
KL, Zand MS. De novo thrombotic microangio-
pathy in renal transplant recipients: a comparison
of hemolytic uremic syndrome with localized renal
thrombotic microangiopathy. Am J Kidney Dis
2003;41:471-9.
10. Pham PT, Danovitch GM, Wilkinson AH et al.
Inhibitors of ADAMTS13: a potential factor in the
cause of thrombotic microangiopathy in a renal
allograft recipient. Transplantation 2002;74:1077-
80.
11. Oyen O, Strom EH, Midtvedt K et al. Calci-
neurin inhibitor-free immunosuppression in renal
allograft recipients with thrombotic microangio-
pathy/hemolytic uremic syndrome. Am J Transplant
2006;6:412-8.
12. Robson M, Cote I, Abbs I, Koffman G, Golds-
mith D. Thrombotic microangiopathy with siro-
limus-based immunosuppression: potentiation of
calcineurin-inhibitor-induced endothelial damage?
Am J Transplant 2003;3:324-7.
13. Egbuna O, Zand MS, Arbini A, Menegus M,
Taylor J. A cluster of parvovirus B19 infections
in renal transplant recipients: a prospective case
series and review of the literature. Am J Transplant
2006;6:225-31.
14. Ki CS, Kim IS, Kim JW et al. Incidence and
clinical signicance of human parvovirus B19
infection in kidney transplant recipients. Clin
Transplant 2005;19:751-5.
15. Barsoum NR, Bunnapradist S, Mougdil
A, Toyoda M, Vo A, Jordan SC.Treatment of
parvovirus B-19 (PV B-19) infection allows for
successful kidney transplantation without disease
recurrence. Am J Transplant 2002;2:425-8.
16. Arzouk N, Snanoudj R, Beauchamp-Nicoud A
et al. Parvovirus B19-induced anemia in renal
transplantation: a role for rHuEPO in resistance to
classical treatment. Transpl Int 2006;19:166-9.
17. Borrows R, Chusney G, Loucaidou M et al.
Mycophenolic acid 12-h trough level monito-
ring in renal transplantation: association with
acute rejection and toxicity. Am J Transplant
2006;6:121-8.
18. Thaunat O, Beaumont C, Chatenoud L et al.
Anemia after late introduction of sirolimus may
correlate with biochemical evidence of a chronic
inammatory state. Transplantation 2005;80:
1212-9.
19. Formica RN Jr, Friedman AL, Lorber MI, Smith
JD, Eisen T, Bia MJ. A randomized trial comparing
losartan with amlodipine as initial therapy for
hypertension in the early post-transplant period.
Nephrol Dial Transplant 2006;21:1389-94.
20. Nosari A, Marbello L, De Carlis LG et al.
Bone marrow hypoplasia complicating tacrolimus
(FK506) therapy. Int J Hematol 2004;79:130-2.
21. Itterbeek P, Vandenberghe P, Nevens F et al.
Aplastic anemia after transplantation for non-
A, non-B, non-C fulminant hepatic failure: case
report and review of the literature. Transpl Int
2002;15:117-23.
22. Sanchez R, Rosenthal P, Goldsby R. Immu-
notherapy for severe aplastic anemia following
orthotopic liver transplantation in children. Pediatr
Blood Cancer 2006; [Epub ahead of print].
23. Snanoudj R, Beaudreuil S, Arzouk N et al.
Recovery from pure red cell aplasia caused by
anti-erythropoietin antibodies after kidney trans-
plantation. Am J Transplant 2004;4:274-7.
24. Pawarode A, Fine DM, Thuluvath PJ. Inde-
pendent risk factors and natural history of renal
dysfunction in liver transplant recipients. Liver
Transpl 2003;9:741-7.
25. Gonwa TA, Mai ML, Klintmalm GB. Chronic
renal failure after transplantation of a nonrenal
organ. N Engl J Med 2003;349:931-40.
26. Smith DM, Agura E, Netto G et al. Liver
transplant-associated graft-versus-host disease.
Transplantation 2003;75:118-26.
27. Taylor AL, Gibbs P, Sudhindran S et al. Monitoring
systemic donor lymphocyte macrochimerism to aid
the diagnosis of graft-versus-host disease after liver
transplantation. Transplantation 2004; 77:441-6.
28. Yanaga K, Tzakis AG, Shimada M et al. Reversal
of hypersplenism following orthotopic liver trans-
plantation. Ann Surg 1989;210:180-3.
29. Barcena R, Gil-Grande L, Moreno J et al.
Partial splenic embolization for the treatment of
hypersplenism in liver transplanted patients with
hepatitis C virus recurrence before peg-interferon
plus ribavirin. Transplantation 2005;79:1634-5.
30. Pillebout E, Nochy D, Hill G et al. Renal
histopathological lesions after orthotopic
liver transplantation (OLT). Am J Transplant
2005;5:1120-9.
 6
6
1
/
6
100%