Immunosenescence et CMV Vaccins et vieillissement

Immunosénescence
et CMV,
Vaccins et
vieillissement
DPML: Mise à jour diagnostique
Autour du vieillissement :
Laboratoire et bilan biologique
Pascal Meylan, Institut de
Microbiologie et Service des
Maladies Infectieuses

agenda
•Le système immunitaire et son vieillissement
• Vieillissement et infections
• Cytomegalovirus, biologie et impact sur le
système immunitaire
•CMV et mortalité
•CMV, immunosénescence, et vaccins
•CMV et maladies cardiovasculaires
• conclusions

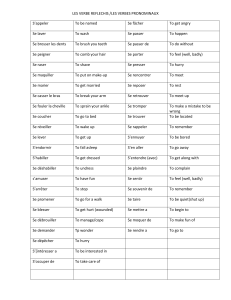
Le système immunitaire et son
vieillissement
D’après Lang et al, NPG, 2012;12:171, Panda et al, J Immunol, 2010; 184:2518, Mitchell et al, Clin Exp
Immunol , 2010;161:497,
1) TLR
2) Output thymique
4) Spent
lymphocytes
3) Répertoire appauvri
5) inflamm-aging

Vieillissement et infections: les
exemples bien connus
•Liés à une baisse documentée de
l’immunité
–Réactivation tuberculeuse
–Zona (réactivation de VZV)
–Listériose
•Liés à une baisse de l’immunité et/ou
d’autres lignes de défense
–Pneumonie
–Infection urinaire

Vieillissement et infections: une
relation quantitative
Curns AT et al, Arch Int Med, 2005;
All cause
ID
 6
6
 7
7
 8
8
 9
9
 10
10
 11
11
 12
12
 13
13
 14
14
 15
15
 16
16
 17
17
 18
18
 19
19
 20
20
 21
21
 22
22
 23
23
 24
24
 25
25
 26
26
 27
27
 28
28
 29
29
1
/
29
100%