Télécharger l'article au format PDF

L’Encéphale (2008) 34, 584—588
Disponible en ligne sur www.sciencedirect.com
journal homepage: www.elsevier.com/locate/encep
SANTÉ PUBLIQUE
Troubles de santé mentale, recours aux soins et au
soutien social chez une population vulnérable :
l’exemple des centres maternels de Paris
Mental Health disorders, medical care and social
support in a vulnerable population: The example of
the maternal centres in Paris
T. Saïasa,∗, T. Greacena, D. Brengardb, M. Lejoyeuxc, M. Bourdaisd
aLaboratoire de recherche de l’établissement public de santé Maison-Blanche, 3—5, rue Lespagnol, 75020 Paris, France
bSecteur 3 de psychiatrie infanto—juvénile de Paris, établissement public de santé Maison-Blanche, France
cSecteur 22 de psychiatrie de Paris, établissement public de santé Maison-Blanche, France
dCellule santé de la sous-direction aux affaires familiales et éducatives, Direction de l’action sociale,
de l’enfance et de la santé (DASES), Paris, France
Rec¸u le 2 mai 2007 ; accepté le 22 janvier 2008
Disponible sur Internet le 19 mai 2008
MOTS CLÉS
Psychopathologie ;
Épidémiologie ;
Précarité ;
Accès aux soins ;
Soutien social ;
Centres maternels
Résumé L’effet pathogène de la précarité sociale sur la santé mentale a fait l’objet de nom-
breuses publications internationales. Ces recherches mettent en valeur la fréquence accrue des
problèmes de santé mentale chez les populations pauvres, sans emploi ou sans domicile. Ce
risque est par ailleurs majoré en période périnatale, où l’incidence des troubles psychologiques
est plus importante qu’à n’importe quel autre moment de la vie. Chez de jeunes mères en situa-
tion de vulnérabilité sociale, l’accès aux réseaux médico-sociaux et à leur réseau de soutien
social est donc primordial. Cette étude consiste en un état des lieux sur les ressources profes-
sionnelles et informelles en santé mentale dont bénéficient les femmes accueillies au sein des
centres maternels de Paris. Quatre-vingt-quinze sujets ont participé à la recherche. Soixante-
huit pour cent d’entre elles validaient un trouble de santé mentale au jour de l’enquête. Parmi
celles-ci, 97 % avaient cherché un recours spécifique pour ce(s) trouble(s) auprès de profes-
sionnels et/ou de leur réseau social. Les forts taux de satisfaction par rapport au soutien rec¸u
démontrent la capacité de cette population à engager un processus fonctionnel de demande
d’aide. En outre, ils mettent en valeur que l’enjeu ne réside pas tant dans la mise en place
∗auteur correspondant.
Adresse e-mail : [email protected] (T. Saïas).
0013-7006/$ — see front matter © L’Encéphale, Paris, 2008.
doi:10.1016/j.encep.2008.01.003

Troubles de santé mentale et recours aux soins chez une population vulnérable accueillie en centre maternel 585
de solutions que dans la nécessité de favoriser l’élaboration de liens entre professionnels de
santé mentale et travailleurs sociaux.
© L’Encéphale, Paris, 2008.
KEYWORDS
Psychopathology;
Epidemiology;
Social deprivation;
Access to care;
Social Support;
Mother-child centers
Summary
Introduction. — The negative effect of social deprivation and poverty on mental health has been
the subject of numerous publications since the 1960s, with studies generally showing a higher
prevalence of mental health disorders in homeless, unemployed or low income populations.
Women in perinatal contexts are also at greater risk for psychopathology: the relative risk for
being hospitalised is up to 60% higher in the perinatal period than during the two years preceding
pregnancy. Access to social care and informal support is therefore particularly important for
pregnant women in vulnerable social conditions. In France, socially excluded mothers access
shelter and accommodation in maternal centres. Over the last few years, staff in these centers
report what they perceive to be as an increase in the prevalence of mental health problems in
the mothers using these services. The current study, CEMAT, set out to examine this question.
Methodology. — Based on a participatory research method, a qualitative and epidemiological
study was carried out in order to evaluate the reality and needs in terms of mental health care
in this population, as well as to evaluate available care and support networks. The study took
place in 2005. All stakeholder groups in six maternal centres agreed to participate in focus
groups and, in addition, residents were invited to respond to epidemiological and qualitative
questionnaires, including the Mini International Neuropsychiatric Interview (MINI 5.0.0) and its
qualitative questions aimed at evaluating use of medical and social network resources. Overall,
95 women took part in this study, representing 61% of all residents. Subjects were young (64%
under 26) and 57% had been living in their centre for over 12 months.
Results. — A percentage of 68% (N= 65) of the participants were identified as having a mental
health disorder, according to the MINI. Of these 65 women, 55 (85%) had consulted a physician
(mainly general practitioners and gynecologists) during the preceding two months. Ninety seven
per cent of women validating one or more MINI diagnoses had specifically looked for help for
these disorders, 17% seeking only professional help (GP, psychiatrist, psychologist, social worker,
expert in non conventional medicine or traditional care), 23%looking for an informal source of
support (partner, family, friends) and 57% using both professional care and informal support.
High rates of satisfaction (69% for professional services, 81% for informal support) showed the
capacity of this population to request relevant social and medico-social support.
Discussion. — Results tend to confirm the links between psychosocial vulnerability and mental
health disorders. On the other hand, the women’s ability to ask for and to access specific
psychological care, whether it be from professionals or informally from friends and family is to
be underlined. The high satisfaction rates tend to prove that, though psychologically vulnerable,
this population has coping capacities that should be recognized and valorized. Options open
to such structures do not necessarily involve the sole development of internal mental health
resources, but need to acknowledge and strengthen existing support networks.
© L’Encéphale, Paris, 2008.
Introduction
La relation entre la psychiatrie et la précarité sociale fait,
depuis les années 1960, l’objet d’études soutenues dans le
champ de la santé mentale [2,10]. Les enquêtes menées
en population générale montrent que, d’une manière géné-
rale, les problèmes de santé mentale et en particulier
la dépression, sont plus fréquents dans les populations
pauvres, sans emploi ou sans domicile [3,5,7,8,10]. Cette
vulnérabilité est d’autant plus importante dans un contexte
périnatal : le risque relatif pour une femme d’être hos-
pitalisée en milieu psychiatrique dans les deux ans qui
suivent une naissance est de 1,6 [6]. Les moyens mis
en œuvre pour faciliter une prise en charge adaptée
sont en constant développement et les populations les
plus précarisées ont vu leurs ressources en santé men-
tale augmenter. Toutefois, le repérage de la souffrance
psychologique des populations dont la vulnérabilité psy-
chosociale est moindre, faute de visibilité, serait moins
systématique.
Les jeunes mères en situation de vulnérabilité psychoso-
ciale se voient offrir sur l’ensemble du territoire franc¸ais
un accueil en centre maternel. Selon les textes, la mission
des ces centres est mixte, visant non seulement l’accueil et
l’hébergement de ces femmes mais également la réinsertion
sociale et le soutien au développement de la parentalité.
Le Département de Paris accueille ainsi 300 femmes en
centre maternel, au titre du dispositif de protection de
l’enfance. Selon Donati et al. [4], seule source d’information
récente sur le profil psychosocial des résidentes des centres
maternels, la vulnérabilité des femmes accueillies est carac-
térisée d’une part par leurs conditions de vie (76 % d’entre
elles vivaient dans un logement précaire avant d’accéder
au centre: hébergement par des tiers, hébergement social,
d’urgence ou de fortune) et d’autre part par l’absence
d’insertion professionnelle, 77 % étant par exemple sans tra-

586 T. Saïas et al.
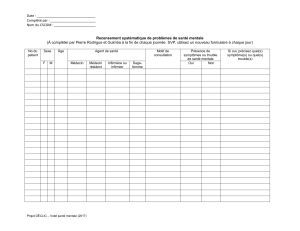
Tableau 1 Résultats de l’étude épidémiologique.
Trouble validé au MINI Centres
maternels (%)
Femmes 18—35 ans,
population générale
(%)
Odd ratios Intervalle de
confiance 95 %
Khi-2 (p)
Épisode dépressif actuel
(dernières deux semaines) (F32)
48 14 5,89 3,91—8,85 p= 0,000
Épisode dépressif récurrent (F33) 28 7 5,03 3,19—7,94 p= 0,000
Risque suicidaire léger 32 11 3,75 2,41—5,82 p= 0,000
Anxiété généralisée (F411) 34 15 2,82 1,83—4,33 p= 0,000
vail. Par ailleurs, on remarque une diversité croissante des
origine ethniques des femmes accueillies [4].
Depuis quelques années, ces structures font état de
ce que le personnel perc¸oit comme un accroissement des
troubles psychiques, voire psychiatriques, parmi les rési-
dentes. La direction de l’action sociale, de l’enfance et de
la santé (DASES) de Paris, tutelle de ces centres, a ainsi
demandé en 2005 la réalisation d’une étude visant à exa-
miner cette situation. Les résultats épidémiologiques et
qualitatifs de cette enquête permettent d’apporter un éclai-
rage sur la question de la psychologisation de l’intervention
sociale [12] et sur le recoupement des missions de chaque
professionnel dans ces institutions.
Méthodologie
L’étude CEMAT a été réalisée d’août à octobre 2005, auprès
du personnel et des femmes accueillies. 95 résidentes de six
centres maternels parisiens ont ainsi été rencontrées. Il leur
était proposé de répondre à un questionnaire épidémiolo-
gique, le Mini International Neuropsychiatric Interview (MINI
5.0.0), ainsi qu’à sa fiche complémentaire et certaines ques-
tions qualitatives investiguant le recours aux soins, pour les
personnes validant au moins un trouble de santé mentale.
Sujets
Les 95 sujets acceptant de participer à la recherche repré-
sentaient 61 % de la capacité d’accueil des six centres
participants. Les sujets rencontrés étaient des femmes
majoritairement jeunes (64 % avaient moins de 26 ans).
57 % des participantes étaient hébergées dans le centre
depuis plus d’un an. Afin de vérifier la représentativité de
l’échantillon, deux variables (âge et durée de séjour) ont
été comparées aux données disponibles pour la totalité de
la population présente en centres maternels. Les résultats
aux tests de Khi-2 ne faisaient pas état de différences signi-
ficatives.
Mesures
Le MINI est un instrument validé en France [9] et capable
de fournir une évaluation diagnostique des symptômes cli-
niques sur la base de la classification internationale des
maladies de l’Organisation mondiale de la santé (CIM-10).
Dans l’étude actuelle, l’administration du MINI a été suivie
par celle de sa fiche complémentaire, permettant d’obtenir
une représentation de l’utilisation du système de soins par
le sujet confronté à un trouble de santé mentale.
Traitement des données
Les données ont été traitées avec le logiciel statistique SPSS
14.0©. Les statistiques descriptives et les tests Khi-2 ont été
utilisés pour l’analyse des variables catégorielles.
Résultats
Résultats épidémiologiques
La recherche épidémiologique a permis de mettre en valeur
une prévalence élevée de troubles de santé mentale. Ainsi
68 % des résidentes interrogées présentaient un diagnostic
psychiatrique actuel, tel qu’investigué par le MINI, la pré-
valence sur la vie entière étant de 78 % pour l’ensemble
des troubles. Ces données ont été comparées avec les don-
nées des femmes de 18 à 35 ans de l’enquête Santé mentale
en population générale, réalisée en 2004 (N= 6827) [1,11].
Cette comparaison révèle que la prévalence des troubles
chez les femmes accueillies en centre maternel est signi-
ficativement plus élevée sur les troubles suivants : épisode
dépressif actuel, épisode dépressif récurrent, risque suici-
daire léger, anxiété généralisée (Tableau 1).
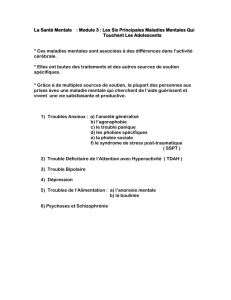
Parmi les facteurs socio-démographiques, seul l’âge
semble influencer ces résultats, notamment en ce qui
concerne la prévalence de troubles anxieux( Tableau 2).
Accès aux soins médicaux
Plus de huit participantes sur dix (82 %, N= 78) avaient
consulté un médecin durant les deux derniers mois (omni-
praticien et gynécologue principalement). Parmi les 68 %
(N= 65) des participantes validant un trouble de santé men-
tale au moment de l’enquête, ce taux d’accès aux soins
Tableau 2 Troubles anxieux par catégorie d’âge.
Oui (%) Non (%) Odd ratios Intervalle de
confiance 95 %
18—21 31 69
22—25 69 31 4,89 1,65—14,47
26—29 50 50 2,20 0,64—7,55
>29 50 50 2,20 0,67—7,22

Troubles de santé mentale et recours aux soins chez une population vulnérable accueillie en centre maternel 587
Tableau 3 Type de recours utilisés par les participantes
présentant un trouble de santé mentale.
Type de recours utilisé % de participantes
Réseau personnel (amis, famille,
conjoint)
80,0
Un psychiatre/Un psychologue 38,5
Un médecin/Des médicaments 38,5
Une hospitalisation (hôpital
général ou psychiatrique)
23,1
Des médecines douces 15,4
Un travailleur social 13,8
Un traitement traditionnel 4,6
Un religieux 3,1
médicaux dans les huit dernières semaines reste inchangé
(85 %, N= 55, ns.).
Recours aux services de santé mentale
Pour chaque participante validant au moins un trouble au
MINI, il lui était demandé si elle avait recherché de l’aide
pour faire face à ce(s) trouble(s). Parmi les participantes
validant un trouble actuel de santé mentale, 97 % avaient
recherché un recours spécifique pour leur problème, 75 %
ayant recherché l’aide d’au moins deux personnes.
Parmi celles ayant recherché une aide, 17 % avaient solli-
cité le seul recours d’un professionnel (médecin, psychiatre,
psychologue, travailleur social, expert en médecines douces
ou traitements traditionnels), 23 % avaient sollicité le seul
recours de leur réseau de soutien social (famille, conjoint,
amis) et 57 % avaient sollicité à la fois leur réseau de soutien
social et des professionnels (Tableau 3).
Le degré de satisfaction par rapport à l’aide rec¸ue était
également étudié. Les résultats, s’ils témoignent d’une
satisfaction générale par rapport à l’aide rec¸ue, sont néan-
moins différents selon la source de l’aide. Si 69 % des
participantes ayant consulté un professionnel se disaient
ainsi satisfaites, ce chiffre montait à 81 % pour le soutien
informel (Tableau 4).
Discussion
Les résultats de cette recherche confirment les liens étroits
entre précarité et troubles de santé mentale. Si la pré-
valence des troubles anxio-dépressifs est importante dans
notre échantillon, le nombre de recours sollicités spontané-
ment par les femmes accueillies est également à remarquer.
La satisfaction qui en découle témoigne des capacités de
cette population à engager un processus fonctionnel de
demande d’aide. Si de nombreux professionnels ont fait état
dans cette recherche de leur inquiétude par rapport à la
gestion des troubles de santé mentale au sein même des
centres maternels, les résultats montrent que la prise en
charge de ces troubles existe, d’une manière plus ou moins
formelle, à l’extérieur de ces structures sociales. L’enjeu ne
réside donc plus tant dans la mise en place de solutions que
dans l’intégration de celles-ci dans la pratique éducative et
dans le travail en réseau avec les professionnels extérieurs
Tableau 4 Satisfaction à l’égard du soutien rec¸u.
Type de soutien/Avec ce soutien,
votre problème s’est...
Arrêté Amélioré Sous-ensemble
«positif »(%)
Pas de
changement
Aggravé Sous-ensemble «neutre
ou négatif »(%)
Non-réponse Total
Un travailleur social 0 9 100 0 0 0 0 9
Réseau personnel (amis, famille,
conjoint)
4 60 81 14 0 18 1 79
Une hospitalisation (hôpital
général ou psychiatrique)
012 71 5 0 29 0 17
Un médecin/Des médicaments 0 19 66 8 0 28 3 29
Un traitement traditionnel 0 2 66 0 0 — 1 3
Un psychiatre/Un psychologue 0 20 59 10 1 32 3 34
Des médecines douces 0 4 36 6 0 55 1 11
Un religieux 0 0 — 0 0 — 2 2
NB : plusieurs réponses possibles pour chaque trouble investigué.

588 T. Saïas et al.
mais aussi avec la famille, les amis et le conjoint de ces
femmes.
La reconnaissance et le développement de ce travail de
terrain, hors les murs de l’institution, ainsi que le dévelop-
pement de groupes de pairs, favoriseraient la redéfinition
des enjeux, dans le cadre d’une politique générale de pro-
motion de la santé mentale. L’intégration de différents
acteurs et de différents modes de soutien psychologique et
social, ainsi que la prise en compte et la reconnaissance des
compétences et des ressources (notion d’empowerment) des
sujets accueillis dans ces institutions dont la mission n’est
pas sanitaire, doivent être favorisées. Il s’agit de mettre
en place de nouvelles manières de collaborer, entre tra-
vail social, prise en charge médicale et soutien social non
professionnel.
Remerciements
Cette recherche a été intégralement financée par la DASES
de Paris (SERD 2004/07/T). Les auteurs tiennent à remer-
cier le Dr P. Leloher et L. Hounkpatin pour leur participation
en tant que membres du comité scientifique, Mmes C. Gold-
ner et P. Tessier, psychologues, qui ont réalisé le recueil des
données, ainsi que l’ensemble des équipes et des résidentes
des centres maternels de Paris ayant accepté de participer
à l’étude.
Références
[1] Bellamy V., Roeland, J., Caria, A., Troubles mentaux et
représentations de la santé mentale : premiers résultats de
l’enquête Santé mentale en population générale [Mental disor-
ders and mental health representations: firsts results of the
French general population study on mental health]. DRESS:
Études et résultats, 2004: 347.
[2] Bhui K, Shanahan L, Hardig G. Homelessness and mental ill-
ness: A literature review and a qualitative study of perceptions
of the adequacy of care. Int J Soc Psychiatry 2006;52(2):
152—65.
[3] Bocognano A, Dumesnil S, Frerot L, et al. Santé Soins et Pro-
tection Sociale en 1998. Paris: CREDES; 1999.
[4] Donati P, Mollo S, Norvez A, et al. Les centres maternels:
réalités et enjeux éducatifs [maternal centers: realities and
educative stakes]. Paris: L’Harmattan; 1999.
[5] Huxley P, Evans S. Social science and mental health. J Ment
Health 2003;12(6):543—50.
[6] Kendell R, McGuire R, Connor Y, et al. Mood changes in the
first three weeks after childbirth. J Affect Disord 1981;3(4):
317—26.
[7] Kovess V. Précarité et santé mentale. In: Références en Psy-
chiatrie. Paris: Doin; 2001.
[8] Le Pape A, Lecomte T. Aspects socio-économiques de la dépres-
sion : Évolution 1980/81—1991/2. Paris: CREDES; 1996.
[9] Lecrubier Y, Sheehan D, Weiller E, et al. The Mini Internatio-
nal Neuropsychiatric Interview (M.I.N.I.), a short diagnostic
Interview: Reliability and validity according to the CIDI. Eur
Psychiatry 1997;12:232—41.
[10] Patel V, Kirkwood B, Pednekar S, et al. Risk factors for com-
mon mental disorders in women. Br J Psychiatry 2006;189:
547—55.
[11] Roelandt J, Caria A, Mondière G. La santé mentale en
population générale : images et réalités. Présentation géné-
rale de l’enquête [mental health in general population:
representations and reality]. L’Information Psychiatrique
2000;76(3):279—92.
[12] Saïas T, Greacen T. Réussir la psychologisation de l’intervention
sociale. In: Bresson M, editor. La psychologisation de
l’intervention sociale : mythes et réalités. Paris: L’Harmattan;
2006. Collection Logiques sociales.
1
/
5
100%