Patient Engagement Project - St

PatientEngagementProject
CancerCareProgram
CancerCareProgram
St.Mary’s Hospital Centre – Quality of Care & Research Symposium
April 25, 2012

DisclosureStatement
•Wehavenoaffiliationsnorany
financialintereststhatwouldposea
conflictofinterest.

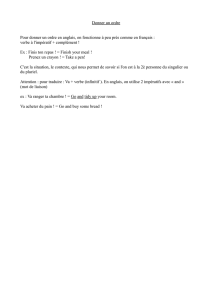
Programmed’orientation
Origineduproblème
•Nospatientsnereçoiventpastouslamême
informationsurlesservicesetlesfaçonsde
faireduprogramme
•Certainspatientsontdesbesoinsnoncomblés
parmanqued’information
•Sentimentdepertedecontrôleaumomentdu
diagnostique
•Augmentationdessentimentsdestresset
d’anxiété
•Perceptiond’allerversl’inconnu,sentiment
d’êtredésorienté

Programmed’orientation
Sesobjectifs
•Redonnerdupouvoirauxpatientsenleuroffrantde
l’informationgénéralesurlecancer,sestraitementset
lagestiondessymptômes.
•Diminuerlessentimentsd’anxiété etdestressliésala
pertedecontrôleenlesfamiliarisantavecl’équipe
soignante,lesservicesetleprogramme.
•Outillernotreclientèleafind’améliorerleurimplication
auniveaudeleursoins.

Leprogrammed’orientationen
bref
•Unerencontredegroupede1haniméeparun
membreduprogrammedeCancérologie.
•Présentationd’uncourtvidéosurlecircuitdu
patientauCentredeJourdeCancérologie.
•PrésentationPowerPoint:Plusieursthèmes
sontabordés
•Documentationécriteremise
 6
6
 7
7
 8
8
 9
9
 10
10
 11
11
 12
12
 13
13
 14
14
 15
15
 16
16
 17
17
 18
18
 19
19
 20
20
 21
21
 22
22
 23
23
 24
24
 25
25
 26
26
1
/
26
100%