http://neurology.thelancet.com Vol 6 January 2007
63
Review
Neurological gait disorders in elderly people: clinical
approach and classifi cation
Anke H Snijders, Bart P van de Warrenburg, Nir Giladi, Bastiaan R Bloem
Gait disorders are common and often devastating companions of ageing, leading to reductions in quality of life and
increased mortality. Here, we present a clinically oriented approach to neurological gait disorders in the elderly
population. We also draw attention to several exciting scientifi c developments in this specialty. Our fi rst focus is on
the complex and typically multifactorial pathophysiology underlying geriatric gait disorders. An important new
insight is the recognition of gait as a complex higher order form of motor behaviour, with prominent and varied
eff ects of mental processes. Another relevant message is that gait disorders are not an unpreventable consequence of
ageing, but implicate the presence of underlying diseases that warrant specifi c diagnostic tests. We next discuss the
core clinical features of common geriatric gait disorders and review some bedside tests to assess gait and balance. We
conclude by proposing a practical three-step approach to categorise gait disorders and we present a simplifi ed
classifi cation system based on clinical signs and symptoms.
Introduction
Gait disorders are common in elderly populations and
their prevalence increases with age. At the age of 60 years,
85% of people have a normal gait, but at the age of
85 years or older this proportion has dropped to 18%.1,2
Gait disorders have devastating consequences. Perhaps
the most notorious corollary is falling, which is often
caused by an underlying gait problem. Injuries caused by
accidental falls range from relatively innocent bruises to
major fractures or head trauma. Another important
consequence is reduced mobility, which leads to loss of
independence. This immobility is often compounded by
a fear of falling, which further immobilises patients and
aff ects their quality of life.3 Importantly, gait disturbances
are also a marker for future development of cardiovascular
disease and dementia.4–6 These associations suggest that
gait disturbances—even when they present in isolation—
can refl ect an early, preclinical, underlying cerebrovascular
or neurodegenerative disease. Finally, gait disorders are
associated with reduced survival, which can be attributed
to a combination of fatal falls, reduced cardiovascular
fi tness, and death from underlying disease.7–9
Elderly patients regularly present with complex gait
disorders, with concurrent contributions from multiple
causal factors.10 To describe specifi c gait disorders
accurately is often diffi cult. Here, we provide a practical
approach that may support clinicians in their everyday
management of neurological gait disorders in elderly
people. We briefl y address the pathophysiology of gait
disorders and discuss the eff ects of mental function and
normal ageing on gait. We conclude by describing a
practical clinical approach and simplifi ed classifi cation
system to diff erentiate gait disorders in everyday practice,
based on clinically discernable gait patterns. Treatments
for geriatric gait disorders are not reviewed.
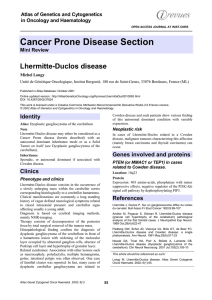
Pathophysiology of gait disorders
Normal gait requires a delicate balance between various
interacting neuronal systems (fi gure 1) and consists of
three primary components: locomotion, including
initiation and maintenance of rhythmic stepping;
balance; and ability to adapt to the environment.
Dysfunction in any of these systems can disturb gait.
Most ambulatory problems in elderly people are caused
by concurrent dysfunction of multiple systems.
Virtually all levels of the nervous system are needed for
normal gait.11–14 Recent studies have drawn attention to
pattern generators in the spinal cord that generate
rhythmic stepping.15 Neuroimaging studies point to the
role of the frontal cortex in controlling gait and in
coordinating automatic and voluntary movements.16 One
interesting study used functional MRI to identify patterns
of brain activity while participants imagined standing,
walking, or running while lying in the scanner.17 With
running (automated locomotion), spinal pattern
generators and the cerebellum were involved, whereas
slow walking evoked activity in the parahippocampal
region, presumably because spatial navigation becomes
more important.
Gait and mental function
Walking is traditionally seen as an automatic motor task
that requires little, if any, higher mental functions. In the
past decade, new insights have drawn attention to the
importance of cognition in daily walking.18 Normal
walking requires strategic planning of the best route, as
well as continuous interaction with the environment and
with internal factors. Failing to understand the signifi cance
of an obstacle, choosing an inappropriate route, or
misinterpreting one’s own physical abilities can all lead to
falls. The safety and effi cacy of normal walking rely not
only on sensorimotor systems, but also critically depend
on the interaction between the executive control
dimension (integration and decision of action) with the
cognitive dimension (eg, navigation, visuospatial
perception, or attention) and the aff ective dimension
(mood, cautiousness, and risk-taking). A common situ-
ation where such an integration is challenged is when
people must walk while performing one or more
secondary tasks. Lundin-Olsson and colleagues19 were
Lancet Neurol 2007; 6: 63–74
Department of Neurology and
Parkinson Center Nijmegen,
Radboud University Nijmegen
Medical Centre, Nijmegen,
Netherlands (A H Snijders MD,
B P van de Warrenburg MD,
B R Bloem MD); and Movement
Disorders Unit, Parkinson
Center, Department of
Neurology, Tel-Aviv Sourasky
Medical Center, Sackler School
of Medicine, Tel-Aviv
University, Tel-Aviv, Israel
(N Giladi MD)
Correspondence to:
Dr Bastiaan R Bloem, Medical
Director, Parkinson Center
Nijmegen (ParC), Department of
Neurology, Radboud University
Nijmegen Medical Centre,
PO Box 9101, 6500 HB
Nijmegen, Netherlands

64
http://neurology.thelancet.com Vol 6 January 2007
Review
the fi rst to note the signifi cance of a failure to maintain
a conversation while walking (“stop walking while
talking”) as a marker for future falls. The ability to
maintain normal walking while performing a secondary
task (dual task paradigm) has become the classic way to
assess the interaction between cognition and gait.20 In
elderly people, this dual task ability deteriorates because
central resources decline, secondary to subclinical disease
processes or medication. This deterioration leads to a
mismatch between the limited personal resources of
elderly people and the complexity of the demand (the
combined walking and secondary task). As a consequence,
elderly people slow down or have an increased stride
variability (suggesting reduced automaticity) while per-
forming a secondary task during walking.21 Gait becomes
less secure and the risk of falling increases. In patients
with overt disease, such as stroke or Parkinson’s disease,
gait deteriorates even more during dual tasking.22–24
Another form of dual task impairment is when elderly
people fail to get their priorities right.25 Under complex
circumstances, young healthy people begin to neglect the
secondary task and lend more priority to walking safely.
This prudent posture-fi rst strategy is diminished in
elderly people,20 and failure to prioritise gait under
diffi cult circumstances is weakly associated with falls.25
Research has shown that frontal executive functions
are especially important for maintaining walking stability.
Dysexecutive functions can be the primary cause of falls
in a group of idiopathic elderly fallers.26,27 The involvement
of cognitive control in normal gait could explain why falls
are so common in patients with dementia and why
demented patients are so vulnerable to dual task
performance while walking.28,29 Interestingly, patients
with Parkinson’s disease whose phenotype is dominated
by postural instability and gait disorder have a much
greater risk of cognitive decline and dementia than do
patients with tremor-dominant Parkinson’s disease.30,31
Additionally, adverse eff ects on cognitive gait control
might explain the high incidence of falls and injuries in
individuals taking psychoactive medication.32
Aff ective disorders are also associated with gait
problems in elderly people. For example, depression,
anxiety, and particularly fear of falling are common
consequences of unsecured gait and falls among elderly
people.33–35
In view of these complex interactions between walking,
cognition, and mood, new interventional strategies
should be developed to promote secured mobility of
elderly people by improving attention, dual task
performance, mood, and executive functions.36
Eff ect of normal ageing on locomotion and gait
Ageing is typically equated with abnormalities, and this
association certainly applies to gait. Many older people
accept their gait diffi culty as being normal for their age
and their doctors often support them in this view. But
are gait disorders truly an inevitable consequence of
ageing itself? This question is illustrated by the evolving
concepts around the so-called senile gait disorder: the
slow, shuffl ing, and cautious walking pattern commonly
seen in older age. Because clinical examination reveals
no apparent cause, normal ageing was long held
responsible for this disorder. However, recent fi ndings
have challenged this concept. Up to 20% of very old
individuals walk normally, hence gait disorders are
certainly not an inevitable feature of old age.1 This
fi nding indirectly implies that those who have
gait impairment in fact suff er from underlying disease.
This assumption is lent support by the fact that
individuals with a senile gait disorder have an increased
risk of becoming demented5 and have reduced survival
compared with age-matched individuals who walk
normally at a high age (fi gure 2).4 These fi ndings
suggest that senile gait disorders are an early
manifestation of underlying pathology, most notably
subtle white-matter changes, vestibular dysfunction,
visual changes, or oculomotor changes.37–43 Such
Feedback:
Vestibular system
Visual system
Sensory nerves
Execution:
Frontal cortex
planning
Basal ganglia
initiation, automatisation
Brainstem
integration
Cerebellum
coordination, adaptation
Spinal cord
spinal pattern generators
Nerve roots
Peripheral nerves
(both motor and sensory)
Muscles
Support:
Cardiovascular system
Bones
Joints
Ligaments
Feet
Figure 1: Levels of the central and peripheral nervous system required for normal gait

http://neurology.thelancet.com Vol 6 January 2007
65
Review
disorders might alter gait directly, but may also act in
an indirect way by causing a subjective sensation of
instability and insecurity, forcing individuals to
purposely adopt a more cautious gait.
The message for clinicians is that gait disorders in
elderly people are not merely the unpreventable
consequence of ageing. Instead, these gait disturbances
more likely result from the increased prevalence and
severity of (clinical or subclinical) diseases with increasing
age (fi gure 3). For this reason, we suggest abandoning
the term senile gait as a specifi c gait category.
Diff erentiation of gait disorders
Only few studies describe the distribution of geriatric
gait disorders. Obviously, the spectrum of underlying
illnesses will depend on the population under
consideration and the assessment technique. Within a
relatively healthy subgroup of 153 community residents
aged 88 years and older, about 61% reported distinct
diseases as a cause of gait impairment.1 Non-neurological
disorders were the leading causes of gait impairment, in
particular joint pain (52 of 87 people), whereas many
others had multiple causes for their gait impairment.
Stroke was the most common neurological cause. In
another study of 120 elderly outpatients seen in a
neurological reference practice, the most common causes
for gait disorders were sensory ataxia (18%), myelopathy
(17%), multiple strokes (15%), and parkinsonism (12%).2
Largely the same causes dominated in a series of 493
neurological inpatients, 60% of whom had a gait
disorder.44
Recognition of specifi c gait disorders
Table 1 summarises the main features of the weak,
spastic, and ataxic gait disorders (for reviews, see
references 13,15,45,46). Because these categories usually cause
little diffi culty in clinical practice, we focus next on the
remaining gait disorders.
Hypokinetic-rigid gait disorders
Diseases of the basal ganglia and the frontal lobe mostly
present with a hypokinetic-rigid gait. However, frontal
pathology can also cause a higher level gait disorder in
which truncal imbalance and frequent falls are a key
feature. Other associated features of this higher level gait
disorder are depression, frontal release signs, and
impaired executive function.47 Specifi c features of gait,
posture, or balance can assist in the diff erential diagnosis
of these diff erent disorders (table 2). A characteristic
feature of hypokinetic-rigid gait is shuffl ing with a
reduced step height, often with a reduced stride length,
leading to slowness of gait. The base of support is typically
normal in Parkinson’s disease, but is often widened in
patients with atypical parkinsonism. Other characteristic
features include reduced arm swing (asymmetrical in
Parkinson’s disease, but more symmetrical in atypical
parkinsonism), which can present in isolation and
precede the onset of other hypokinetic-rigid features by
many years. Turning movements become slow and are
executed en bloc. Festination is a feature of more
advanced disease, where patients take rapid small steps
in an attempt to maintain the feet beneath the forward
moving trunk. Poorly mobile patients with advanced
disease can sometimes respond quickly to environmental
events—typically emotional or threatening circum-
stances—and move unexpectedly well (kinesia para-
doxica). Apparently, patients with Parkinson’s disease
0123456
Survival (years)
0·0
0·2
0·4
0·6
0·8
1·0
Cumulative survival
Normal gait
Senile gait disorder
Gait disorder due to disease
Figure 2: Kaplan-Meier curves showing cumulative survival due to all causes of death
Results are shown for patients with a completely normal gait (n=25), those with senile gait disorders (n=14), and
those with gait disorders due to known disease (n=87). Mean age was 90 years in all groups (range 87–97 years).
Survival was diff erent between the groups (log-rank p=0·01). All-cause-mortality risk was increased in people with
senile gait disorders compared with those with a normal gait (RR=2·8; 95% CI 1·1–7·3, p = 0·03) and was similar to
those with gait disorders due to known disease (RR=1·2; 95% CI 0·6–2·5, p=0·6). Mortality due to cardiovascular
disease also diff ered among the three groups, with a two-fold increased risk of cardiovascular death in people with
senile gait disorders compared with those with normal gait (data not shown). Reproduced with permission from
Blackwell Publishing.4
Gait disorders
Ageing
Falls
Injuries
Mortality
Immobility Reduced quality
of life
Age-related
pathology
Fear of
falling
Morbidity
(cardiovascular disease,
cognitive decline)
?
Figure 3: Indirect association between ageing and geriatric gait disorders
This association occurs mainly, if not exclusively, via the intermediate of age-related pathology. Adverse
consequences of gait disorders in elderly people include reduced quality of life and, eventually, reduced survival.

66
http://neurology.thelancet.com Vol 6 January 2007
Review
can use such external triggers to engage alternative motor
circuits and thereby bypass the defective basal ganglia
circuitry.48
Hypokinetic-rigid gait disorders can be classifi ed
according to the underlying anatomical substrate. One
main group involves lesions within the basal ganglia and
their connections to the frontal cortex, brainstem, or
both. Pathological changes in the frontal lobe itself can
also contribute to a hypokinetic-rigid gait. There are no
well-defi ned clinical markers for frontal-lobe contribution,
but suggestive features include a wide-based or variable
stance and truncal imbalance. Some would also include
gait apraxia here, often defi ned as a marked discrepancy
between the severity of the gait disorder and the ability to
perform other leg movements, such as cycling in the air
while lying down. Associated features include urinary
urgency and cognitive changes and a poor response to
external cues.
Hypokinetic-rigid gait disorders can also be classifi ed
according to the underlying disease process. One
important group includes neurodegenerative disorders
such as Parkinson’s disease and various forms of atypical
parkinsonism (eg, multiple system atrophy or progressive
supranuclear palsy). Another common group includes
underlying cerebrovascular disease. Gait disorders with a
mixed hypokinetic-rigid and ataxic character are a
common occurrence in patients with subcortical
arteriosclerotic encephalopathy.49 A less common feature
of cerebrovascular disease is lower body parkinsonism, a
predominance of symptoms and signs in the legs, with a
relatively preserved arm swing and little bradykinesia of
the hands.50,51 The term lower body parkinsonism is a
useful descriptive term in clinical practice because it
refers to a recognisable phenotype that is often associated
with underlying cerebrovascular disease, including white-
matter changes and lacunar infarcts in the basal ganglia.
However, lower-body parkinsonism is not synonymous
with vascular parkinsonism. Occasional patients can
present with a clinical presentation resembling
Parkinson’s disease (with upper-limb involvement) or
even progressive supranuclear palsy. Hypokinetic-rigid
gait disorders due to cerebrovascular disease can develop
acutely or with an insidious onset.50 The acute syndrome
mainly involves infarcts in the putamen, globus pallidus,
or thalamus, whereas the gradual form is associated with
diff use white-matter changes.
A third type of underlying disease process is ventricular
widening, as occurs in patients with normal pressure
Elements of the clinically based diagnostic work-up
Main features of gait Specifi c gait or balance test* Associated symptoms and signs
Antalgic gait Reduced stance phase on aff ected limb
Limping
Pain
Limited range of movements
Paretic/hypotonic gait High steppage
Dropping foot
Waddling
Trendelenburg’s sign Lower motor neuron features (eg, weakness,
atrophy, low to absent tendon refl exes)†
Spastic gait Circumduction
Intermittent abduction of ipsilateral arm with each step
Foot dragging: audible “scuffi ng toe”
Scissoring; bilateral circumduction
Pyramidal syndrome
Anterior-medial side of the shoe sole worn out
Vestibular gait Deviation to one side Aggravated by eye closure
Positive Unterberger test
Vestibular features (eg, nystagmus, abnormal
tilting test)
Sensory ataxic gait Staggering, wide based Aggravated by eye closure Disturbed proprioception
Cerebellar ataxic gait Staggering, wide based Not aggravated by eye closure Cerebellar ataxia (eg, dysarthria, hypermetria,
nystagmus)
Dyskinetic gait Extra movements that aff ect gait Can be task-specifi c (eg, dystonic gait) Features of dystonia, chorea, myoclonus or tics
Hypokinetic-rigid gait Shuffl ing (slow speed, short stride, rigidity, reduced step height)
Hesitation and freezing
Improves with external cues
Aggravation by secondary task
Hypokinetic-rigid features (eg, bradykinesia,
resting tremor)
Cautious gait “Walking on ice”; slow, wide base, short steps
Striking improvement with external support
Postural instability (mild to moderate)
Excessive fear of falling
Higher level gait disorder Severe balance impairment (no rescue reactions with the
pull test; “falling like a log”)
Inadequate synergies
Inappropriate or bizarre foot placement
Crossing of the legs
Leaning into wrong direction when turning or standing
Variable performance (infl uenced by environment
and emotion)
Hesitation and freezing (ignition failure)
Abnormal interaction with environment (eg, trouble
adapting with walking aids; no benefi t from cues)
Sometimes better able to perform cycling leg
movements while recumbent (gait “apraxia”)
Frontal release signs
Executive dysfunction
Depression
Frequent falls
A clinically based diagnosis for each gait syndrome can usually be reached with a systematic approach: fi rst, a description of the core gait features; next, the use of specifi c gait or balance tests; and fi nally, a search
for associated symptoms and signs. *Simple diagnostic tests that can be done at the bedside include: providing external support (eg, a walking aid); imposing secondary tasks while walking (dual or multiple
tasking); eye closure; walking backwards; infl uence of external cues (visual; auditory; or mental). †Peripheral neuropathy and radiculopathy are among the most common causes of gait diffi culties in the elderly.
Table 1: Main features of specifi c gait syndromes

http://neurology.thelancet.com Vol 6 January 2007
67
Review
hydrocephalus. Whether normal pressure hydrocephalus
truly exists as a separate entity with its own unique
pathophysiology is unknown. Typically, the disorder
presents with a recognisable triad of hypokinetic-rigid
gait impairment, urinary incontinence, and (frontal)
dementia. Gait is characterised by marked slowing and
small shuffl ing steps and regular freezing, but usually
with largely preserved arm movements.52,53 Ataxic
elements are also seen, including a broad stance width
and an increased variability in timing and amplitude of
the steps. The pathophysiology has not been clarifi ed,
but may relate to an excessive volume of intraventricular
cerebrospinal fl uid that is not explained by cerebral
atrophy. The classic radiological appearance includes
widened lateral ventricles (especially aff ecting the
anterior horns), often accompanied by periventricular
white-matter lesions. An unresolved question (yet one
with direct implications for treatment) is whether these
periventricular white-matter lesions are the cause or
consequence of ventricular widening.54
Clinical examination alone cannot always disentangle
these diff erent anatomical and pathophysiological causes
of hypokinetic-rigid gait disorders, especially in early
stages where overlap is substantial. In such patients, it is
best to refrain from confusing terminology. It initially
suffi ces to classify the patient as having a hypokinetic-
rigid gait disorder and to base a more defi nitive
anatomical or aetiological diagnosis on ancillary
investigations (MRI) and sometimes the response to
treatment (eg, a trial of levodopa).
Cautious and careless gaits
Typically, people with a cautious gait move slowly, with a
wide base and short strides, with little movement of the
trunk, while the knees and elbows are bent. Cautious gait
is common in elderly people and originates in part from
fear of falling, which is sometimes present to the degree of
panic.33 There are two main subgroups. In the fi rst, fear of
falling is excessive relative to the degree of actual instability.
In fact, balance can be fully normal, as in people with a
Main anatomical substrate Disease process Characteristic features Associated features
Parkinson’s disease (PD) Substantia nigra Neurodegenerative Narrow-based gait
Asymmetrical presentation
Stooped posture
Early freezing and falls rare
Good response to
levodopa
Resting tremor hand(s)
Multiple system atrophy,
parkinsonian type
Basal ganglia
Cerebellum
Pyramidal tracts
Autonomic nervous system
Neurodegenerative Early phase like PD gait
Later phase more wide-based
Pisa syndrome
Antecollis
Vertical falls (due to syncope)
Cerebellar ataxia
Autonomic features
Pyramidal signs
Progressive supranuclear
palsy
Diff use brainstem pathology Neurodegenerative Wide-based gait
Freezing common
Erect posture, but with retrocollis
Early/spontaneous/backward falls
Motor recklessness
Frequent and severe injuries
Vertical gaze palsy
Pseudobulbar palsy
Frontal dementia
Applause sign
Corticobasal degeneration Basal ganglia
Cortex
Neurodegenerative Asymmetrical presentation—eg, unilateral
leg apraxia, dystonia, or myoclonus
Later: wide-based gait, freezing, shuffl ing
Apraxia
Alien limb
Cortical sensory loss
Dementia with Lewy bodies Basal ganglia
Cortex
Neurodegenerative Like PD gait
More symmetric
Dementia
Fluctuations
Visual hallucinations
Subcortical arteriosclerotic
encephalopathy
Subcortical white matter Vascular Small steps
Wide-based gait
Start hesitation
Variable timing and amplitude of steps
Urinary incontinence
Cognitive decline
Stepwise progression
Vascular parkinsonism Diff use white matter
Basal ganglia
Vascular Lower body parkinsonism
More wide based
Less stooped
Relatively preserved arm swing
Urinary incontinence
Cognitive decline
Stepwise progression
Strategic vascular lesion Putamen
Globus pallidus
Thalamus
Dorsal mesencephalon
Vascular Lower body parkinsonism
Freezing/severe gait akinesia
Severe disequilibrium
Drifting to one side
Normal pressure
hydrocephalus
Frontostriatal (periventricular) Ventricular widening Wide-based gait, freezing, gait apraxia
Truncal imbalance
Preserved arm swing
Urinary incontinence
Cognitive decline
Drug-induced parkinsonism Basal ganglia (postsynaptic) Mild gait impairment, rarely freezing
Preserved postural refl exes
Pisa syndrome
Upper limb tremor
Symmetrical presentation
Table 2: Diff erential diagnosis of parkinsonian disorders, based on specifi c features of gait, balance, or posture
 6
6
 7
7
 8
8
 9
9
 10
10
 11
11
 12
12
1
/
12
100%