The Mini-Mental State Examination:
pitfalls and limitations
Emma Devenney,
1,2,3
John R Hodges
1,4
1
Frontier, Neuroscience Research
Australia, Sydney, Australia
2
Prince of Wales Clinical School,
University of New South Wales,
Sydney, Australia
3
Brain and Mind Centre,
University of Sydney,
Sydney, Australia
4
School of Medical Sciences,
University of New South Wales,
Sydney, Australia
Correspondence to
Dr Emma Devenney,
Neuroscience Australia, Barker
Street, Randwick, Sydney 2035,
Australia; e.devenney@neura.
edu.au
Accepted 6 November 2016
To cite: Devenney E,
Hodges JR. Pract Neurol
Published Online First: [please
include Day Month Year]
doi:10.1136/practneurol-
2016-001520
The Mini-Mental State Examination
(MMSE) first appeared in 1975 having
been developed as a screening tool for
patients with dementia and psychiatric
disorders in an inpatient setting.
1
Folstein
and colleagues did not envisage the
global domination that this simple clinical
tool would achieve. They clearly state in
their seminal paper that ‘the MMS
cannot be expected to replace a complete
clinical appraisal in reaching a final diag-
nosis in any individual patient’. But, as
frequently happens, this major caveat was
quickly forgotten, and, over the course of
the next 40 years, this brief 30-item
examination gained immense fame
among clinicians as a quick and easy
method to diagnose dementia. The
MMSE is strongly influenced by non-
cognitive domains; it does not reliably
translate across cultures, as the results are
likely to be confounded by language,
levels of literacy, and cultural and ethical
norms. Despite this, the MMSE has been
translated into numerous languages
including Cantonese, Arabic, Spanish and
Persian.
23
Furthermore, it is unreliable
for patients with less than 5 years of edu-
cation, probably because of the heavy
weighting on language and mathematical
abilities. A quick search through the
120 000 references related to the MMSE
on PubMed quickly reveals these pitfalls,
yet it continues to be the cornerstone of
dementia diagnosis in many clinical
rooms throughout the world.
The MMSE has a role in diagnosing
‘barn door’, well-established dementia
and in monitoring patients with moderate
dementia, but many clinicians are still
unaware of its limitations, even in a
Western culture. It has been repeatedly
shown that the MMSE is poor at identi-
fying early-stage dementia, especially
mild cognitive impairment: such a patient
may have severe amnesia and yet score
in the normal range on the MMSE.
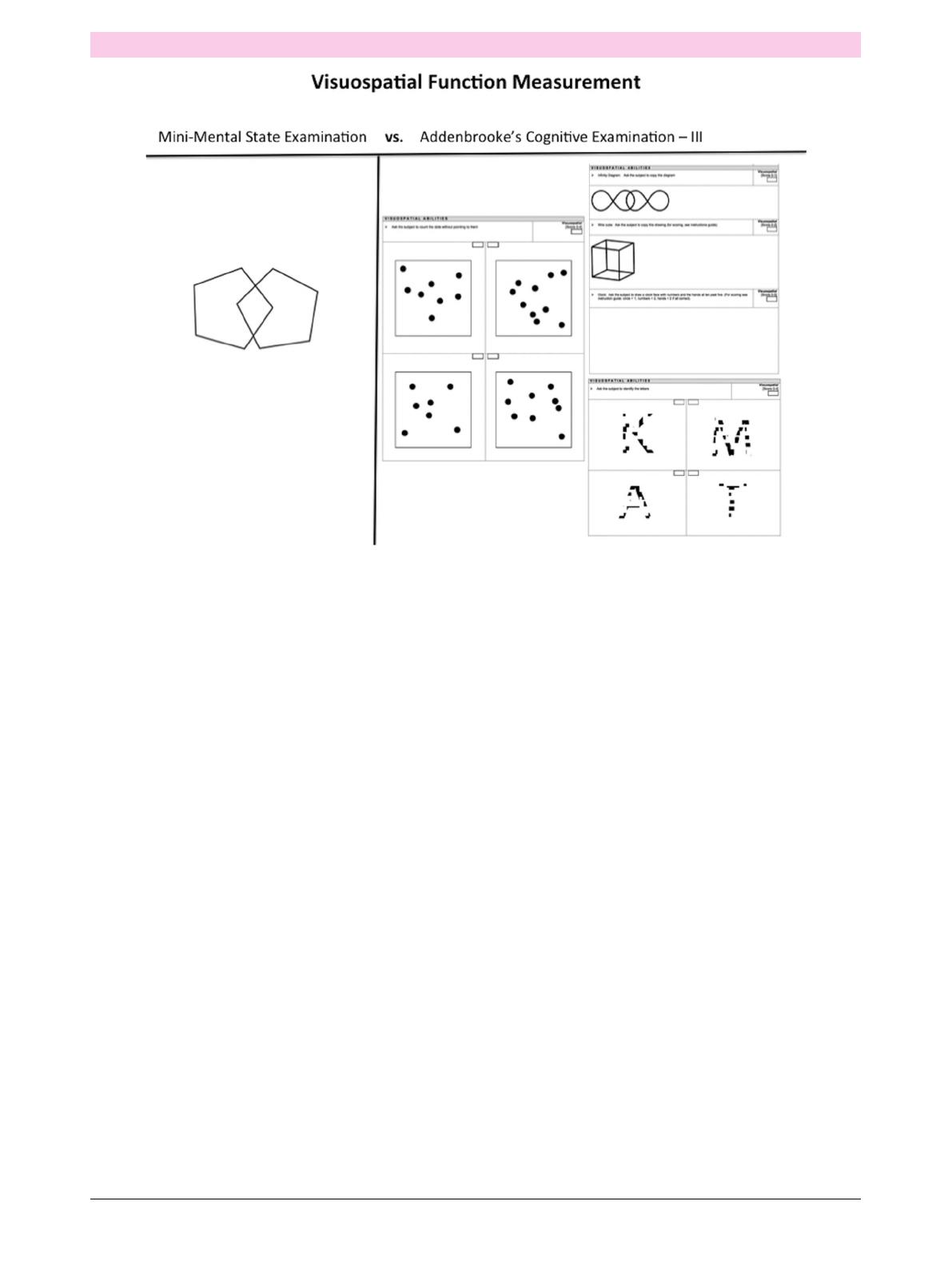
Other worrying features are the lack of
components sensitive to executive func-
tion and the reliance on just one item
(the overlapping pentagons) to screen for
visuospatial deficits (figure 1). The
MMSE is particularly feeble in assessing
patients with frontotemporal dementia,
many of whom score within the ‘normal’
range on the test yet cannot function
in social or work situations. Another
slightly longer test is the Addenbrooke’s
Cognitive Examination, now in its third
incarnation (ACE-III); it takes 15–20 min
to administer and is used to screen for
mild cognitive impairment, frontotem-
poral dementia and other less common
causes of dementia.
45
In this modern technological era,
where medical diagnoses often rely
heavily on a combination of highly
complex investigations, it seems unthink-
able that the diagnosis of a devastating
illness such as Alzheimer’s disease would
hinge on the results of a rough-and-ready
5 min test, the answers to which the
patient spent the last 45 min rehearsing
in the car on the way to the appointment.
Never mind the fact that mood, educa-
tion status and ethnicity could heavily
influence the results. Perhaps even more
concerning is that an equally devastating
illness such as frontotemporal dementia
could be completely missed because the
executive and emotional deficits often
experienced by patients early in the
disease course are not examined by a
restrictive tool that measures only the
basic memory, attention, language and
visuospatial functions.
There is clearly a need to update prac-
tice and, while recognising the MMSE’s
contribution to dementia, it is high time
it retired gracefully to make room for
newer, more theoretically motivated and,
importantly, free assessment tools in
dementia. Fortunately, there are now
several superior assessment tools available
for use in the clinic that can be supported
by neuropsychological assessment and,
NEUROMYTHOLOGY
Devenney E, Hodges JR. Pract Neurol 2016;0:1–2. doi:10.1136/practneurol-2016-001520 1
when this is inconclusive, by brain imaging. However,
the issue of which type of imaging is another story.
Contributors ED and JRH contributed to the conception and
design of the work and drafting and revising the manuscript;
they approve the final version and agree to be accountable for
the work.
Funding This work was supported by funding to Forefront, a
collaborative research group dedicated to the study of
frontotemporal dementia and motor neurone disease, from the
National Health and Medical Research Council of Australia
programme grant (No 1037746) and the Australian Research
Council Centre of Excellence in Cognition and its Disorders
Memory Node (No CE110001021). ED is supported by a
UNSW PhD scholarship and the Motor Neurone Disease
Association UK.
Competing interests None declared.
Provenance and peer review Commissioned. Externally peer
reviewed. This paper was reviewed by Martin Rossor, London,
UK.
REFERENCES
1 Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”:a
practical method for grading the cognitive state of patients for
the clinician. J Psychiatr Res 1975;12:189–98.
2EspinoDV, Lichtenstein MJ, Palmer RF, et al.Ethnicdifferences
in mini-mental state examination (MMSE) scores: where you
live makes a difference. J Am Geriatr Soc 2001;49:538–48.
3 Escobar JI, Burnam A, Karno M, et al. Use of the mini-mental
state examination (MMSE) in a community population of
mixed ethnicity. Cultural and linguistic artifacts. J Nerv Ment
Dis 1986;174:607–14.
4 Hsieh S, Schubert S, Hoon C, et al. Validation of the
Addenbrooke’s cognitive examination III in frontotemporal
dementia and Alzheimer’s disease. Dement Geriatr Cogn
Disord. 2013;36:242–50.
5 Mathuranath PS, Nestor PJ, Berrios GE, et al. A brief cognitive
test battery to differentiate Alzheimer’s disease and
frontotemporal dementia. Neurology 2000;55:1613–20.
Figure 1 Comparison of the components used to screen for visuospatial deficits in the Mini-Mental State Examination and the
Addenbrooke’s Cognitive Examination –III.
NEUROMYTHOLOGY
2Devenney E, Hodges JR. Pract Neurol 2016;0:1–2. doi:10.1136/practneurol-2016-001520
1
/
2
100%