http://cid.oxfordjournals.org/content/36/9/e107.full.pdf

BRIEF REPORT •CID 2003:36 (1 May) •e107
BRIEF REPORT
Epstein-Barr Virus and Human
Herpesvirus 8 Coinfection and
Concomitant Extranodal Nasal-Type
NK/T Cell Lymphoma and Castleman
Disease: Case Report
Claire Larroche,
1
Fe´lix Agbalika,
2
He´le`ne Poirel,
3
Antoine Martin,
4
Agne`s Gautheret-Dejean,
5
Martine Raphae¨l,
3
and Olivier Lortholary
1
Departments of
1
Internal Medicine and Infectious Disease and
3
Biological
Hematology and
4
Pathology Laboratory, Hoˆpital Avicenne, Universite´ Paris–Nord,
Bobigny,
2
Department of Virology, Hoˆpital Saint-Louis, and
5
Department of
Virology, Hoˆpital Pitie´-Salpe´trie`re, Paris, France
We describe a 36-year-old man uninfected with human im-
munodeficiency virus who had confirmed concurrent infec-
tion with Epstein-Barr virus (EBV) and human herpesvirus
8 (HHV-8) and their respective lymphoproliferative mani-
festations, nasal-type NK/T cell lymphoma and Castleman
disease. Antibodies to HHV-8 and EBV DNA were found in
plasma and peripheral blood mononuclear cells. An EBV-
positive nasal-type NK/T cell lymphoma infiltrated the
splenic red pulp, whereas the white pulp contained HHV-
8–positive plasmablasts, as found in Castleman disease.
Multicentric Castleman disease (CD), primary effusion lym-
phoma, and Kaposi sarcoma are 3 diseases associated with hu-
man herpesvirus (HHV)-8 infection that occur in HIV-infected
and HIV-uninfected patients. HHV-8 and Epstein-Barr virus
(EBV) coinfection is well known in immunosuppressed pa-
tients, such as HIV-positive persons with primary effusion lym-
phoma [1], and was recently reported anecdotally in an infant
with primary immunodeficiency [2]. Herein we describe a case
of EBV and HHV-8 coinfection with the concomitant lym-
phoproliferative disorders, nasal-type NK/T cell lymphoma and
CD, respectively, in an HIV-uninfected man.
Received 2 October 2002; accepted 12 December 2002; electronically published 22 April
2003.
Presented in part: 4th International Conference on Human Herpesviruses 6, 7, and 8, Paris,
10–12 May 2001 (abstract 45).
Reprints or correspondence: Dr. Claire Larroche, Dept. of Internal Medicine and Infectious
Diseases, Hoˆpital Avicenne, 125 Rue de Stalingrad, 93009 Bobigny Cedex, France (claire.
Clinical Infectious Diseases 2003;36:e107–10
2003 by the Infectious Diseases Society of America. All rights reserved.
1058-4838/2003/3609-00E2$15.00
Case report. A 36-year-old man from the Comoro Islands
was hospitalized at Avicenne Hospital (Bobigny, France) for
fever, chills, and weight loss of 1 month’s duration. Physical
examination revealed marked hepatosplenomegaly and jaun-
dice. Blood tests revealed pancytopenia with profound lym-
phocytopenia (leukocyte count, 2900 cells/mm
3
, with 250 lym-
phocytes/mm
3
and a CD4:CD8 ratio of 0.76; hemoglobin level,
8 g/dL; and platelet count, 95,000 cells/mm
3
), inflammatory
syndrome (fibrinogen level, 6.2 g/L, and C-reactive protein
level, 139.5 mg/L), hepatic dysfunction (aspartate aminotrans-
ferase level, 309 IU/L; alanine aminotransferase level, 273 IU/
L; and total bilirubin, 28.6 mM), hypertriglyceridemia (triglyc-
eride level, 6.08 mM; range, 0.50–1.67 mM), a high serum
ferritin level (27,427 ng/mL; range, 30–280 ng/mL), and hy-
ponatremia (Na concentration, 128 mM). Bone marrow as-
pirate and liver biopsy revealed pronounced hemophagocytosis.
The patient tested negative for HIV (by serological test and
PCR) and for human T cell lymphotropic virus 1 (by serological
test). No cytomegalovirus, HHV-6, or HHV-7 replication was
detected. We detected EBV reactivation (IgG and IgM anti-
bodies to viral capsid antigen, IgM to early antigen and IgG to
nuclear antigen), and plasma and PBMCs were strongly positive
for EBV DNA (6.69 log
10
copies/mL and 4.40 log
10
copies/mL,
respectively) and HHV-8 DNA (7.2 log
10
copies/mL and 7.08
log
10
copies/mL, respectively). Anti–HHV-8 latent and lytic an-
tibodies were also detected. Other causes of hemophagocytic
syndrome were excluded. Intravenous immunoglobulintherapy
had no effect. The patient’s clinical status worsened. Because
of severe spleen involvement, a splenectomy was performed,
and intravenous methylprednisolone was prescribed. However,
the patient’s condition deteriorated rapidly, and he died of
multiple-organ failure.
Methods. For analysis of EBV and HHV-8, isolates were
subjected to molecular analysis with quantitative PCR. We an-
alyzed a sample of DNA (1 mg) extracted from PBMC and
plasma fractions by means of the QIAamp Blood Kit (Quiagen)
and used PCR b-globin amplification of DNA samples as con-
trols. We used the Taqman-based technique (Biosystem) of
Kennedy et al. [3] to detect EBV DNA, as described by Kimura
et al. [4], and to detect HHV-8 DNA, as described elsewhere
[5]. Virus load was estimated from standard curves established
from dilutions of DNA from the Namalwa (Burkitt) cell line
(for EBV) and diluted plasmid controls (for HHV-8). Calibra-
tion copy numbers ranged from 10
1.5
to 10
6
for 50 mL(
rp
).0.98–0.99
Standard histological analyses were performed by 2 pathol-

e108 •CID 2003:36 (1 May) •BRIEF REPORT
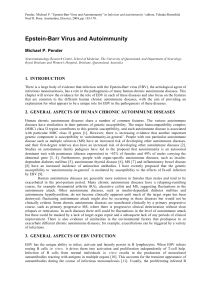
Figure 1. Photomicrographs showing extranodal nasal-type NK/T cell lymphoma in the splenic red pulp. Immunohistological labeling revealed a
sinus containing a dense infiltrate of neoplastic cells that were cytoplasm CD3positive (A) and had membranes reactive with CD8 (B) and TiA1
(C). Epstein-Barr virus (EBV) in situ hybridization revealed that most of the neoplastic cells were positive for EBV-encoded small RNA (D).
ogists. Immunophenotyping was performed with paraffin-
embedded tissue samples taken from the spleen, liver, and bone
marrow with use of monoclonal antibodies directed against an
HHV-8 latent nuclear antigen encoded by viral open reading
frame 73 to detect HHV-8 in tissue samples [6]. EBV was
detected by means of in situ hybridization with fluorescein
isothiocyanate-labeled, EBV-encoded small RNA (EBER) 1⫹2-
specific oligonucleotides (EBER in situ hybridization [ISH];
Dako), according to the manufacturer’s instructions [7].
Results and discussion. Histological examination of
splenic red pulp specimens identified a dense infiltration of a
mixture of medium-sized and large lymphoid cells with irreg-
ular nuclei. These cells, all of which were EBER positive, had
an immunophenotype consistent with nasal-type NK/T cell

BRIEF REPORT •CID 2003:36 (1 May) •e109
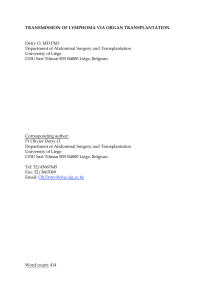
Figure 2. Photomicrographs showing evidence of human herpesvirus (HHV)-8–positive Castleman disease in the splenic white pulp. A, Section
showing a hyalinized germinal center surrounded by a broad concentric mantle of small lymphocytes, a finding consistent with the diagnosis of CD.
B, At high magnification, small lymphocytes, mature plasma cells, and plasmablasts (arrow) can be seen in the mantle zone. C, Lymphocytes and
plasmablasts were labeled by in situ hybridization with the HHV-8 latent nuclear antigen 1–specific monoclonal antibody.
lymphoma: they were CD3-cytoplasm positive and demon-
strated CD8, CD16, CD56, and TiA1 cell-membrane expression
(figure 1), but they were negative for cell-surface CD5 and CD3
expression. Rare individual lymphoma cells were detected by
EBER ISH of the bone marrow and liver sections. T cell–
receptor genes were in germ-line configuration in PBMCs and
in the spleen specimen. Hyalinized germinal centers sur-
rounded by a broad concentric mantle of small lymphocytes,
mature plasma cells and plasmablasts were seen in splenic
white-pulp follicles and in a hilar splenic lymph node specimen,

e110 •CID 2003:36 (1 May) •BRIEF REPORT
a finding that is consistent with the diagnosis of CD. ISH studies
to detect latent nuclear antigen 1 revealed HHV-8–positive lym-
phocytes and plasmablasts in the mantle zone (figure 2). A few
mature plasma cells were found in the bone marrow and liver,
but CD was diagnosed only on the basis of findings from the
spleen. No HHV-8–positive cells were seen in the liver and
bone marrow specimens. Hemophagocytosis was prominent in
the bone marrow, spleen, and liver specimens.
The most striking point in this case is the simultaneous
lymphoproliferative manifestations of infection with 2 herpes-
viruses in an HIV-negative patient: extranodal nasal-type NK/
T cell lymphoma due to EBV infection and CD due to HHV-
8 infection in the same organ. The coinfection might be a
coincidence, because this man originated from an area (the
Comoro Islands) where HHV-8 is endemic.
The simultaneous presence of EBV and HHV-8 DNA se-
quences in lymphoid tissues was recently described in an HIV-
negative infant with primary immunodeficiency who did not
have lymphoma or CD [2]. Also pertinent is a recent report
of concomitant occurrence of EBV-positive Hodgkin lym-
phoma and HHV-8–positive CD in the same lymph node [8].
In our patient, the EBV-associated nasal-type NK/T cell lym-
phoma was principally located in the spleen, which is indeed
a surprising and extremely rare observation [9]. Of note, it is
known that EBV can establish type 2 latency in cell lines derived
from patients with this type of lymphoma [10]. However, al-
though the EBV-transforming latent membrane protein 1 is
clearly implicated in lymphomagenesis, other transforming
events seem to be necessary [11]. HHV-8 contains a battery of
cellular gene homologues that encode proteins involved in sig-
nal transduction, cell cycle regulation, inhibition of apoptosis,
and/or immune modulation [12]. HHV-8 may act indirectly
through the release of growth factors targeting stroma cells [13].
Therefore, our hypothesis that HHV-8 induced paracrine stim-
ulation, which has been advanced with respect to Kaposi sar-
coma [14], might explain the simultaneous occurrence of CD
and NK/T cell lymphoma in the same lymphoid organ.
References
1. Klepfish A, Sarid R, Shtalrid M, Shvidel L, Berrebi A, Schattner A.
Primary effusion lymphoma (PEL) in HIV-negative patients—adistinct
clinical entity. Leuk Lymphoma 2001; 41:439–43.
2. Sanchez-Velasco P, Ocejo-Vinyals JG, Flores R, Gomez-Roman JJ, Loz-
ano MJ, Leyva-Cobian F. Simultaneous multiorgan presence of human
herpesvirus 8 and restricted lymphotropism of Epstein-Barr virus DNA
sequences in a human immunodeficiency virus-negative immunode-
ficient infant. J Infect Dis 2001; 183:338–42.
3. Kennedy MM, Lucas SB, Jones RR, et al. HHV8 and Kaposi’s sarcoma:
a time cohort study. Mol Pathol 1997; 50:96–100.
4. Kimura H, Morita M, Yabuta Y, et al. Quantitative analysis of Epstein-
Barr virus load by using a real-time PCR assay. J Clin Microbiol
1999; 37:132–6.
5. Oksenhendler E, Carcelain G, Aoki Y, et al. High levels of human
herpesvirus 8 viral load, human interleukin-6, interleukin-10, and C-
reactive protein correlate with exacerbation of multicentric Castleman
disease in HIV-infected patients. Blood 2000; 96:2069–73.
6. Kellam P, Bourboulia D, Dupin N, et al. Characterization of mono-
clonal antibodies raised against the latent nuclear antigen of human
herpesvirus 8. J Virol 1999; 73:5149–55.
7. Barletta JM, Kingma DW, Ling Y, Charache P, Mann RB, Ambinder
RF. Rapid in situ hybridization for the diagnosis of latent Epstein-Barr
virus infection. Mol Cell Probes 1993; 7:105–9.
8. Caussinus E, Meggetto F, Delsol G, Brousset P. Simultaneous occur-
rence of Epstein-Barr virus associated Hodgkin’s disease and HHV-8
related multicentric Castleman’s disease: a fortuitous event? J Clin
Pathol 2001; 54:790–1.
9. Chan JK, Sin VC, Wong KF, et al. Nonnasal lymphoma expressing the
natural killer cell marker CD56: a clinicopathologic study of 49 cases
of an uncommon aggressive neoplasm. Blood 1997; 89:4501–13.
10. Tsuchiyama J, Yoshino T, Mori M, et al. Characterization of a novel
human natural killer-cell line (NK-YS) established from natural killer
cell lymphoma/leukemia associated with Epstein-Barr virus infection.
Blood 1998; 92:1374–83.
11. Cesarman E, Mesri EA. Virus-associated lymphomas. Curr Opin Oncol
1999; 11:322–32.
12. Damania B, Jung JU. Comparative analysis of the transforming mech-
anisms of Epstein-Barr virus, Kaposi’s sarcoma–associated herpesvirus,
and Herpesvirus saimiri. Adv Cancer Res 2001; 80:51–82.
13. Ensoli B, Sturzl M. Kaposi’s sarcoma: a result of the interplay among
inflammatory cytokines, angiogenic factors and viral agents. Cytokine
Growth Factor Rev 1998; 9:63–83.
14. Cesarman E, Mesri EA, Gershengorn MC. Viral G protein-coupled
receptor and Kaposi’s sarcoma: a model of paracrine neoplasia? J Exp
Med 2000; 191:417–22.
1
/
4
100%