Cost Effectiveness of Gene Expression Profiling for Early Stage Breast Cancer

Cost Effectiveness of Gene Expression Profiling for Early Stage
Breast Cancer
A Decision-Analytic Model
Mo Yang, MS
1,2
; Suja Rajan, PhD
1,2
; and Amalia M. Issa, PhD, MPH
1,2,3
BACKGROUND: Gene expression profiling (GEP) is being used increasingly for risk stratification to identify women with lymph node-
negative, estrogen receptor-positive, early stage breast cancer who are most likely to benefit from adjuvant chemotherapy. The
authors of this report evaluated the cost effectiveness of recurrence score-guided treatment using 2 commercially available GEP
tests, Oncotype DX (Genomic Health, Redwood City, Calif) and MammaPrint (Agendia Inc., Irvine, Calif), from a third-party payer’s
perspective. METHODS: A 10-year Markov model was developed to compare the costs and quality-adjusted life-years (QALYs) of
treatment decisions guided by either Oncotype DX or MammaPrint in a hypothetical cohort of women with early stage, lymph node-
negative, estrogen receptor-positive breast cancer who may experience recurrence. Outcomes included no recurrence, recurrence,
and death. The costs considered included gene test costs, the costs of adjuvant chemotherapy and other chemotherapy (including
premedication, oncology visits, and monitoring for adverse events), the cost of treating recurrence, costs associated with the treat-
ment of adverse events, and end-of-life care costs. RESULTS: The model demonstrated that the patients who received the Oncotype
DX test to guide treatment spent $27,882 (in US dollars) and gained 7.364 QALYs, whereas patients who received the MammaPrint
test to guide treatment spent $21,598 and gained 7.461 QALYs. Sensitivity analyses demonstrated that the results were robust to
changes in all parameters. CONCLUSIONS: The model suggested that MammaPrint is a more cost-effective GEP test compared with
Oncotype DX at a threshold willingness-to-pay of $50,000 per QALY. Because Oncotype DX is the most frequently used GEP in clini-
cal practice in the United States, the authors concluded that the current findings have implications for health policy, particularly
health insurance reimbursement decisions. Cancer 2012;118:5163–70. V
C2012 American Cancer Society.
KEYWORDS: gene-expression profiling, breast cancer, Markov modeling, cost-effectiveness, health economics.
INTRODUCTION
Breast cancer is the second most common malignancy and the second most common cause of cancer death for women in
the United States. Breast cancer accounts for an estimated 209,060 newly diagnosed cases annually.
1
A key challenge for
patients with breast cancer and their health care providers while making treatment decisions relates to the decision to use
or forego adjuvant chemotherapy.
2,3
The argument for the use of adjuvant chemotherapy is the potential to reduce the
risk of recurrence and mortality for patients with breast cancer. However, there is variation in the degree of benefit from
adjuvant therapy, and the benefit is questionable for patients who have estrogen receptor-positive, or lymph node-nega-
tive, or tamoxifen-responsive disease.
4-6
Chemotherapy also is expensive for payers and may produce significant toxicities,
such as myelosuppression and permanent ovarian failure, which may have a substantial impact on quality of life.
4
Several gene expression profiling (GEP) assays are currently on the market for use as genomic diagnostics to provide
prognostic or risk information. The potential value of these genomic diagnostics lies in their claims to measure gene
expression levels of a patient’s tumor and to produce a ‘‘numerical score’’ depicting risk for disease recurrence. The estima-
tion of disease recurrence helps identify patients who are likely to benefit from chemotherapy and, thus, assists providers
in making decisions regarding the administration of chemotherapy. However, these tests differ from one another in several
ways, including the presentation of risk recurrence data.
To date, Oncotype DX (Genomic Health, Redwood City, Calif), a 21-gene profile assay that uses real-time (RT) po-
lymerase chain reaction (PCR) for expression analysis of paraffin-embedded tissue, remains the most frequently used GEP
in clinical practice in the United States. Oncotype DX uses a recurrence score (RS), which places patients in 3 categories:
high risk, intermediate risk, and low risk. The putative test objective is to tailor treatment to the individual patient so that
DOI: 10.1002/cncr.27443, Received: September 18, 2011; Revised: November 23, 2011; Accepted: December 6, 2011, Published online February 22, 2012 in
Wiley Online Library (wileyonlinelibrary.com)
Corresponding author: Amalia M. Issa, PhD, MPH, Program in Personalized Medicine and Targeted Therapeutics and Department of Health Policy and Public
Health, University of the Sciences, 600 S. 43rd Street, Box 22, Philadelphia, PA 19104; Fax (215) 596-7614; a.issa@usciences.edu
1
Program in Personalized Medicine and Targeted Therapeutics, University of the Sciences, Philadelphia, Pennsylvania;
2
Department of Clinical Sciences and
Administration, College of Pharmacy, University of Houston, Houston, Texas;
3
Department of Health Policy and Public Health, University of the Sciences, Philadel-
phia, Pennsylvania.
Cancer October 15, 2012 5163
Original Article

patients with a low risk of recurrence who do not need
chemotherapy can avoid it, which will enhance patient
quality of life and save money for payers.
MammaPrint (Agendia Inc., Irvine, Calif), a 70-
gene profile microarray assay that was developed and is
used more frequently in Europe, reports results in a binary
mode: either high risk or low risk for recurrence. Mam-
maPrint uses fresh-frozen tumor tissues, which are avail-
able more frequently from procedures done in Europe,
whereas Oncotype DX uses tissues preserved in paraffin, a
typical procedure in the United States.
Two trials with the expressed purpose of examining
efficacy and providing level I evidence of Oncotype DX
and MammaPrint, the Trial Assigning Individualized
Options for Treatment (TAILORx) and the Microarray
in Lymph node-Negative Disease may Avoid Chemother-
apy (MINDACT) trial, respectively, currently are
ongoing.
7-9
However, full results from those trials are not
yet available, and decisions regarding quality of life and
costs need to be made in the interim.
Although previous economic analyses have been
conducted on GEP assays,
10-17
to our knowledge, only 1
study examined MammaPrint,
13,17
and we are not aware
of any studies that have compared the cost-effectiveness of
these 2 commercially available GEPs directly. The use of
GEP may have significant effects on patient outcomes,
medical services use, and costs. Much of the discussion
surrounding health care reform before and after the enact-
ment of the Patient Protection and Affordable Care Act
18
is centered on ways to create higher quality, more efficient
care and to reduce rising health care expenditures. Thus,
assessing the outcomes, use, and costs associated with
these genomic diagnostic tests is critical for future clinical
decision making. The objective of the current study was
to evaluate the cost effectiveness of treatment decisions
using Oncotype DX compared with treatment decisions
using MammaPrint from a third-party payer’s
perspective.
MATERIALS AND METHODS
Model Description
A 10-year Markov model was developed using Tree-Age
(TreeAge Software, Williamstown, Mass) to evaluate the
costs and quality-adjusted life-years (QALYs) associated
with using 2 GEP-guided treatment strategies: Oncotype
DX and MammaPrint. Patients were distributed into 3
mutually exclusive health states: no recurrence (disease-
free survival), recurrence, and death. The study was con-
ducted from a third-party payer’s perspective.
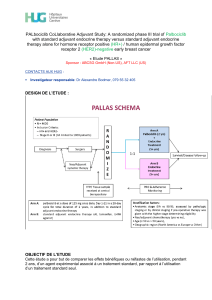
The model assumed a hypothetical cohort of 1000
patients with lymph node-negative, estrogen receptor-
positive breast cancer and simulated events for receiving
either of the 2 GEP tests (Fig. 1). All patients started with
a risk classification state based on an assessment by Adju-
vant! Online (Adjuvant, Inc., San Antonio, Tex). Subse-
quently, patients were reclassified into risk categories
based on the 2 GEP tests using reclassification probabil-
ities from the literature.
15,17,19-22
We compared each of
the 2 GEP tests with Adjuvant! Online, because both
strategies had been compared previously for analytic vali-
dation purposes with Adjuvant! Online in earlier stud-
ies.
17,19-21
In the first strategy, patients were offered
Oncotype DX, and their risk was reclassified using the RS.
For the second strategy, patient risk was reclassified
according to MammaPrint.
We assumed that each patient could only have 1 re-
currence. Once a patient enters a health state, the patient
will not progress to a better health state. A total simulated
time horizon of 10 years was conducted with 1 year con-
sidered as a cycle. During each Markov cycle, the patients
may remain disease-free or develop recurrence. Once
patients develop recurrence, they remain in the recurrence
state until they die from breast cancer. Costs and QALYs
are discounted at 3% in the base case. Patients may experi-
ence no, minor, major, or fatal toxicity from chemother-
apy. We also assumed that 90% of patients who were at
high risk according to both Adjuvant! Online and Onco-
type DX received chemotherapy, whereas 90% of patients
who were at low risk according to both Adjuvant! Online
and Oncotype DX did not receive chemotherapy. For
patients who experienced a conflicting result between Ad-
juvant! Online and Oncotype DX, 50% of the subpopula-
tion received chemotherapy. The same assumption was
applied to MammaPrint.
Probability of Risk Classification
Data on risk classification using Adjuvant! Online and
GEP tests were derived from the literature (Table 1).
15,22
For Strategy 1, in total, 668 patients were classified as ei-
ther low risk or high risk using Adjuvant! Online, and
they were reclassified as low risk or high/intermediate risk
using the RS. The intermediate-risk group was combined
with the high-risk group in the RS category. Of the 354
patients (52.99%) at low risk according to Adjuvant!
Online, 216 (61.02%) were reclassified as low risk, and
138 (39%) were reclassified as high risk using the RS. Of
the 314 patients (47.01%) at high risk according to Adju-
vant! Online, 122 (38.85%) were reclassified as low risk,
and 192 (61.15%) were reclassified as high risk using the
RS. For Strategy 2, in total, 302 patients were classified as
Original Article
5164 Cancer October 15, 2012

either low risk or high risk using Adjuvant! Online, and
they were reclassified as low risk or high risk using Mam-
maPrint.
18
Of the 80 patients (26.58%) at low risk
according to Adjuvant! Online, 52 (65%) were reclassified
as low risk, and 28 (35%) were reclassified as high risk
using MammaPrint. Of the 222 patients (73.51%) at
high risk according to Adjuvant! Online, 59 (26.58%)
were reclassified as low risk, and 163 (73.42%) were
reclassified as high risk using MammaPrint.
Risk of Recurrence and Death
Model inputs for transition probabilities based on recur-
rence rates and death rates for different risk classifications
were obtained from the literature (Table 2).
10,15-18,23
On
the basis of a study by Hornberger et al,
10
a 15% relative
risk reduction in the recurrence rate because of chemo-
therapy was applied to patients classified as high risk by
both Oncotype DX RS and MammaPrint.
10,24,25
A 45%
relative risk reduction in the recurrence rate because of
chemotherapy was applied to patients classified as low risk
by both Oncotype DX RS and MammaPrint.
10,24,25
We
assumed that the transition probability of death was con-
stant. The probabilities of different toxicities after chemo-
therapy were obtained from the literature.
26
Utility
The utility used to adjust survival for quality of life ranges
from 0 to 1, with 0 representing death and 1 representing
perfect health (Table 2). Utilities for toxicity from chemo-
therapy, recurrence-free states, and recurrence states were
obtained from the peer-reviewed literature, including a
systematic review of cost-utility assessment in oncology
and a review of health-related quality-of-life esti-
mates.
27,29
The QALYs were calculated by the length of
time spent in a health state multiplied by the utility of that
state.
Costs
Unit costs were obtained from various sources. All costs
are reported in 2009 US dollars. Costs from a different
Figure 1. The analytical decision model assumed patients with lymph node-negative, estrogen receptive-positive (þ) breast can-
cer for the Oncotype DX (21-gene signature) and MammaPrint (70-gene signature) gene expression profiling tests, and simulated
events for 2 strategies. All patients started in the risk classification state in which they underwent risk assessment by Adjuvant!
Online (Adjuvant, Inc., San Antonio, Tex). In the first strategy, patients were offered Oncotype DX, and their risk was reclassified
using the recurrence score. For the second strategy, patients’ risk was reclassified according to MammaPrint.
Cost-Effectiveness of GEP Tests/Yang et al
Cancer October 15, 2012 5165

base year were inflated by 3% per year. The cost of Onco-
type DX was based on the list price of $3975, whereas the
cost of MammaPrint was $4200.
Costs of chemotherapy included costs for chemo-
therapy medications and administration. We assumed a
threshold willingness to pay for breast cancer of
$50,000, and this was increased to $100,000 for sensi-
tivity analyses. Costs that were considered in the model
are listed in Table 3.
Outcomes
The model generated estimates of the health care costs
and QALYs, incremental cost per QALY gained, and
incremental cost-effectiveness ratio (ICER). The ICER
Table 2. Transition Probabilities and Utilities Used in Modeling the 2 Gene Expression Profiling Strategies
Variable Base Case Range Tested in
Sensitivity Analysis
Reference
Transition probability
Probability of toxicity Hillner & Smith 1991
26
Minor 0.60 0.48-0.72
Major 0.05 0.04-0.06
Fatal 0.005 0.004-0.006
Death rates: Adjuvant! Online/GEP Buyse 2006
19
High/high 0.036 0.027-0.045
High/low 0.012 0.009-0.015
Low/high 0.036 0.027-0.045
Low/low 0.013 0.010-0,016
Utility
No chemotherapy 1.00 0.75-1.00 Assumption
No recurrence with/without chemotherapy 0.98 0.74-1.00 Earle 2000
27
Recurrence with/without chemotherapy 0.75 0.56-0.94 Earle 2000
27
No toxicity from chemotherapy 1.00 — Assumption
Minor toxicity from chemotherapy 0.80 0.60-1.00 Gold 1996
28
Major toxicity from chemotherapy 0.70 0.53-0.88 Gold 1996
28
Death 0 — Assumption
Abbreviations: GEP: gene expression profiling.
Table 1. Risk Reclassification and Recurrence Rates for the Oncotype DX and MammaPrint Gene Expression Profiling Tests
Adjuvant! Online
a
Oncotype DX
b
Comparator
Risk Group
No. of Patients
in Risk Group (%)
10-Year Risk
of Recurrence, %
Risk
Group
No. of Patients in
Risk Group (%)
10-Year Risk
of Recurrence, %
References
Low 354 (52.99) 8.40 Low 216 (61.02) 5.60 Tsoi 2010
15
;
Marchionni 2008
22
Int/high 138 (38.98) 12.85
High 314 (47.01) 22.20 Low 122 (38.85) 8.90
Int/high 192 (61.15) 30.71
Adjuvant! Online MammaPrint
c
Comparator
Risk Group
No. of Patients
in Risk Group
(%)
10-Year Risk
of Recurrence,
%
Risk
Group
No. of Patients
in Risk Group
(%)
10-Year Risk
of Recurrence,
%
References
Low 80 (26.49) 8.40 Low 52 (65) 5.60 Tsoi 2010
15
;
Buyse 2006
19
;
Marchionni 2008
22
High 28 (35) 12.85
High 222 (73.51) 22.20 Low 59 (26.58) 8.90
High 163 (73.42) 30.71
Abbreviations: Int/high, intermediate/high.
a
Adjuvant! Online; Adjuvant, Inc., San Antonio, Tex.
b
Oncotype DX; Genomic Health, Redwood City, Calif.
c
MammaPrint; Agendia Inc., Irvine, Calif.
Original Article
5166 Cancer October 15, 2012

estimated the differences in cumulative costs divided by
the differences in QALYs between the Oncotype DX and
MammaPrint strategies.
Sensitivity Analyses
One-way sensitivity analyses were performed on assump-
tions, probabilities, and costs while holding the other vari-
ables fixed to assess the robustness of the Markov model.
A probabilistic analysis using Monte Carlo simulation was
carried out to determine the effect of uncertainty in all
variables on the cost-utility ratio for the cohort. We
applied the simulation 1000 times to ensure the reliability
of the model. To quantify the uncertainty captured by the
sensitivity analysis, we used 1000 Monte Carlo simula-
tions to perform ttests and establish whether the costs and
effectiveness associated with MammaPrint and Oncotype
DX were statistically different from one another. This
helped establish the statistical robustness of our sensitivity
analysis.
RESULTS
Base-Case Analysis
The model shows that patients for whom Oncotype DX
was used to guide treatment spent US $27,882 and gained
7.364 QALYs, whereas patients for whom MammaPrint
was used to guide treatment spent US $21,598 and gained
7.461 QALYs (Table 4). The results suggest that Mam-
maPrint is a more cost-effective test than Oncotype DX at
a threshold willingness to pay of $50,000 per QALY.
Sensitivity Analyses
Sensitivity analyses were performed using an incremental
cost-effectiveness (ICE) scatter plot between Oncotype
DX versus MammaPrint with 1000 Monte Carlo simula-
tion trials using MammaPrint as the reference category
(Fig. 2). In this plot, each trial point represents a compari-
son of the incremental costs and effectiveness of Mam-
maPrint and Oncotype DX using simultaneous and
randomly assigned values from the probability, costs and
outcome distributions of the base-case parameter esti-
mates. The ICE scatter plot diagram was divided into 4
quadrants. A trial point in Quadrant I indicates that
Oncotype DX is more costly and more effective than
MammaPrint. A trial point in Quadrant II indicates that
Oncotype DX is more costly and less effective than Mam-
maPrint, thereby indicating that MammaPrint the domi-
nant strategy. A trial point in Quadrant III suggests that
Oncotype DX is less costly and less effective than Mam-
maPrint. A trial point in Quadrant IV suggests that Onco-
type DX is less costly and more effective than
Table 3. Costs Used in Modeling the 2 Gene Expression Profiling Strategies
Variable Base Case, $ Range Tested in
Sensitivity Analysis, $
Reference
GEP tests Slodkowska 2009
30
Oncotype DX 3975 2981-4969
MammaPrint 4200 3150-5250
Adjuvant chemotherapy 19,618 14,714-24,523 Hornberger 2005
10
Other chemotherapy costs Elkin 2004
39
Premedication, per cycle 15 11-18
Oncology visit, per cycle 44 33-55
Monitoring for side-effects, per y 668 501-835
Recurrence 10,837 8128-13,546 Hillner & Smith 1991
26
Treatment of side effects Hillner & Smith 1991
26
Minor 2709 2032-3386
Major 18,061 13,546-22,576
Fatal 45,153 33,865-56,441
End-of-life 34,778 26,084-43,473
Abbreviations: GEP: gene expression profiling.
Table 4. Incremental Cost-Effectiveness Ratio Results for the Base Case
Diagnostic
Strategy
Costs, $ Incremental, $ QALYs Incremental QALYs C/E, $/QALYs ICER, $/QALYs
MammaPrint 21,598 7.461 2895
Oncotype DX 27,882 6284 7.364 0.097 3786 Dominated
Abbreviations: C/E, cost-effectiveness; ICER, incremental cost-effectiveness ratio; QALYs, quality-adjusted life-years.
Cost-Effectiveness of GEP Tests/Yang et al
Cancer October 15, 2012 5167
 6
6
 7
7
 8
8
1
/
8
100%