Canadian Oncology Nursing Journal Revue canadienne de soins

Canadian Oncology
Nursing Journal
Revue canadienne
de soins infirmiers
en oncologie
The ofcial publication of the Canadian Association of Nurses in Oncology
La publication ofcielle de l’Association canadienne des inrmières en oncologie
Fall/Automne 2014 ISSN: 1181-912X
Volume 24, No. 4 PM#: 40032385


Canadian Oncology Nursing Journal
Revue canadienne de soins infirmiers en oncologie
A publication of the Canadian Association of Nurses in Oncology—Une publication de l’Association canadienne des infirmières en oncologie
PUBLICATIONS MAIL AGREEMENT NO. 40032385. RETURN UNDELIVERABLE CANADIAN ADDRESSES TO:
Canadian Association of Nurses in Oncology, 375 West 5th Avenue, Suite 201, Vancouver, BC, V5Y 1J6, E-mail: [email protected]
Fall/Automne 2014
Volume 24, No. 4
Articles
Table of Contents/Table des matières
233 Editorial
236 Éditorial
Communiqué
312 President’s message: CANO/ACIO Strategic Directions
2013–2016
313 Message de la présidente : Orientations stratégiques
2013–2016 de l’ACIO/CANO
313 Director at Large—Education
314 Conseillère générale—Éducation
315 Director at Large—Professional Practice
316 Conseillère générale—Pratique professionnelle
317 Complementary Medicine Special Interest Group
321 Groupe d’intérêts spéciaux Pratiques complémentaires
325 DAL—Membership
325 Conseillère générale—
Service aux membres
326 Nurse to know: Shawne Gray
326 Une inrmière qu’il fait bon connaître : Shawne Gray
327 Nurse to know: Shari Moura
329 Une inrmière qu’il fait bon connaître : Shari Moura
331 Nurse to know: Philiz Goh
332 Une inrmière qu’il fait bon connaître : Philiz Goh
Features/Rubriques
237 Patient perspective
239 Perspective d’un patient
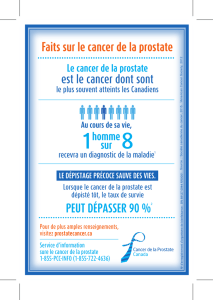
287 Resource review
288 Examen de ressource
289 Ask an ethicist
290 Demandez à un éthicien
291 Book review
292 Critique de livre
293 Resources for patients and family members
294 Ressources pour les patients et leur famille
295 Reections on research
297 Réexions sur la recherche
299 International perspectives
300 Perspectives internationales
302 Quality improvement
306 Amélioration de la qualité
241 Using a web-based decision support intervention to facilitate patient-physician communication at prostate
cancer treatment discussions
by B. Joyce Davison, Michael Szafron, Carl Gutwin, and Kishore Visvanathan
248 Une intervention en ligne de soutien à la décision pour faciliter la communication patient-médecin en lien
avec le traitement du cancer de la prostate
par B. Joyce Davison, Michael Szafron, Carl Gutwin et Kishore Visvanathan
256 A biopsychosocial approach to sexual recovery after prostate cancer treatment: Suggestions for oncology
nursing practice
by Lauren M. Walker, Andrea M. Beck, Amy J. Hampton, and John W. Robinson
264 Une approche biopsychosociale au rétablissement sexuel après le traitement du cancer de la prostate :
suggestions pour la pratique infirmière en oncologie
par Lauren M. Walker, Andrea M. Beck, Amy J. Hampton et John W. Robinson
272 The sexual and other supportive care needs of Canadian prostate cancer patients and their partners:
Defining the problem and developing interventions
by Deborah L. McLeod, Lauren M. Walker, Richard J. Wassersug, Andrew Matthew, and John W. Robinson
279 Les besoins de nature sexuelle et en soins de soutien des Canadiens atteints du cancer de la prostate et de
leurs partenaires : définition du problème et développement des interventions
par Deborah L. McLeod, Lauren M. Walker, Richard J. Wassersug, Andrew Matthew et John W. Robinson

CONJ • RCSIO Fall/Automne 2014
Canadian Oncology Nursing Journal
Revue canadienne de soins infirmiers en oncologie
Canadian Oncology Nursing Journal/Revue canadienne de soins infirmiers en oncologie is a refereed journal.
Editor-in-Chief Margaret I. Fitch, RN, PhD, 207 Chisholm Avenue, Toronto, Ontario M4C 4V9.
Phone: 416-690-0369; Email: [email protected]
Associate Editors Janice Chobanuk, RN, BScN, MN, CON(C)—books/media Jeanne Robertson, RN, B.Arts, BScN, MBA—French materials
Pat Sevean, RN, BScN, EdD—features Sharon Thomson, RN, MSc, BA, MS—manuscript review
Sally Thorne, RN, PhD, FCAHS—research
Reviewers Nicole Allard, RN, MSN, PhD, Bilingual, Maxine Alford, RN, PhD, Karine Bilodeau, inf., PhD(C), French, Joanne Crawford, RN, BScN,
CON(C), MScN, PhD(c), Dauna Crooks, DNSc, MScN, BScN, Jean-François Desbiens, inf., PhD, French, Sylvie Dubois, inf., PhD, Bilingual,
Corsita Garraway, EN(EC), MScN, CON(C), CHPH, Vicki Greenslade, RN, PhD, Virginia Lee, RN, BA, MSC(A), PhD, Bilingual,
Manon Lemonde, RN, PhD, Bilingual, Maurene McQuestion, RN, BA, BScN, MSc, CON(C), Beth Perry, RN, PhD, Karyn Perry, BSN, MBA,
Patricia Poirier, PhD, RN, Dawn Stacey, RN, MScN, PhD, (CON), Jennifer Stephens, RN, BSN, MA, OCN, Pamela West, RN, MSc, ACNP,
CON(C), CHPCN(C), Kathleen Willison, RN, MSc, CVAA(c), CHPCN(c), Patsy Yates, RN, PhD
Managing Editor Heather Coughlin, 613-735-0952, fax 613-735-7983, e-mail: [email protected]
Production The Canadian Oncology Nursing Journal is produced in conjunction with Pappin Communications, The Victoria Centre,
84 Isabella Street, Pembroke, Ontario K8A 5S5, 613-735-0952, fax 613-735-7983, e-mail [email protected], and
Vice Versa Translation, 144 Werra Rd., Victoria, British Columbia V9B 1N4, 250-479-9969, e-mail: [email protected]
Statement The Canadian Oncology Nursing Journal is the official publication of the Canadian Association of Nurses in Oncology, and is
of purpose directed to the professional nurse caring for patients with cancer. The journal supports the philosophy of the national association.
The philosophy is: “The purpose of this journal is to communicate with the members of the Association. This journal currently acts as
a vehicle for news related to clinical oncology practice, technology, education and research. This journal aims to publish timely papers,
to promote the image of the nurse involved in cancer care, to stimulate nursing issues in oncology nursing, and to encourage nurses to
publish in national media.” In addition, the journal serves as a newsletter conveying information related to the Canadian Association
of Nurses in Oncology, it intends to keep Canadian oncology nurses current in the activities of their national association. Recognizing
the value of nursing literature, the editorial board will collaborate with editorial boards of other journals and indexes to increase the
quality and accessibility of nursing literature.
Indexing The Canadian Oncology Nursing Journal/Revue canadienne de soins infirmiers en oncologie is registered with the National Library
of Canada, ISSN 1181-912X, and is indexed in the Cumulative Index to Nursing and Allied Health Literature, (CINAHL), the
International Nursing Index and Medline.
Membership All nurses with active Canadian registration are eligible for membership in CANO. Contact the CANO national office. Refer to the
Communiqué section for name and contact information of provincial representatives.
Subscriptions The journal is published quarterly in February, May, August and November. All CANO members receive the journal. For
non-members, yearly subscription rates are $119.77 (HST included) for individuals, and $131.88 (HST included) for institutions.
International subscriptions are $156.11 (HST included). Payment must accompany all orders and is not refundable. Make cheques
payable to CANO-CONJ and send to the CANO national office. Notices and queries about missed issues should also be sent to the
CANO national office. Canadian Association of Nurses in Oncology, 570 West 7th Avenue, Suite 400, Vancouver, BC V5Z 1B3,
www.cano-acio.ca; telephone: 604-630-5493; fax: 604-874-4378; email: [email protected]
Author Guidelines for authors are usually included in each issue. All submissions are welcome. At least one author should be a
Information registered nurse, however, the editor has final discretion on suitability for inclusion. Author(s) are responsible for acknowledging all
sources of funding and/or information.
Language Policy/ The Canadian Oncology Nursing Journal is officially a bilingual publication. All journal content submitted and reviewed by the editors
Politique will be printed in both official languages. La Revue canadienne de soins infirmiers en oncologie est une publication officiellement
linguistique bilingue. Le contenu proprement dit de la Revue qui est soumis et fait l’objet d’une évaluation par les rédactrices est publié dans les
deux langues officielles.
Advertising For general advertising information and rates, contact Heather Coughlin, Advertising Manager, Pappin Communications, 84 Isabella St.,
Pembroke, Ontario K8A 5S5, 613-735-0952, fax 613-735-7983, e-mail [email protected]. All advertising correspondence and
material should be sent to Pappin Communications. Online rate card available at: www.pappin.com
Opinions expressed in articles published are those of the author(s), and do not necessarily reflect the view of the Canadian Association of Nurses in Oncology or
the editorial board of the Canadian Oncology Nursing Journal. Acceptance of advertising does not imply endorsement by CANO or the editorial board of CONJ.
All rights reserved. The law prohibits reproduction of any portion of this journal without permission of the editor.
Fall/Automne 2014
Volume 24, No. 4

CONJ • RCSIO Fall/Automne 2014 233
As guest editor, I am
excited to be a part of this
first special, themed issue
of CONJ. Our focus here
is on prostate cancer and,
particularly, the sexual and
supportive care challenges,
which are many. It is an area of practice
in which I have been involved for more
than 10 years, as an educator, researcher
and practitioner. During the time that I
have worked with couples affected by
prostate cancer, I have been disturbed
by the ways in which men’s—and their
spouse’s or partner’s—needs have been
poorly and inconsistently addressed by
our health care systems. Very often I
have encountered couples who have suf-
fered silently (or even not so silently) for
years before I see them. They tell me sto-
ries of struggling alone, particularly try-
ing to figure out the sexual challenges,
or of giving up, drifting apart and strug-
gling with depression. The abandonment
of a sexual relationship can lead to a pro-
found loss of intimacy in the relationship
overall for many couples. I have heard
also from many partners who feel com-
pletely overlooked, alone, or even worse,
experience their concerns dismissed
by health care professionals (HCPs). It
seems that HCPs often believe that men
affected by prostate cancer “do well” and
“have few issues”, even with such diffi-
cult treatments as androgen depriva-
tion therapy. Of course, some do; though
many do not, as the articles in this issue
describe.
During my time as a faculty mem-
ber with the Canadian Association of
Psychosocial Oncology’s IPODE (www.
ipode.ca) project, I have also heard
nurses express shock and surprise after
seeing presentations like Ross Gray’s
“No Big Deal” or reading his photo story
“Simon’s Romantic Evening”. One nurse
(who I consider to be an excellent cli-
nician, by the way) told me “After 10
years as an oncology nurse working
with men in this area, I had absolutely
no idea (her emphasis) what they were
going through”. Understandably, she
was distressed, but also, I hope, pro-
pelled to start making changes in her
practice.
Participants in seminar discussions
about sexuality and cancer sometimes
question the need to address sexual
health concerns with this (or other) can-
cer populations. The argument goes
something like this… We are not experts
in sexual health; beyond giving some basic
information I don’t think it is our role to
be “sex therapists”. There are experts
in the community who can do this.” To
this, I offer a couple of responses. First,
the sexual health problems that peo-
ple encounter after cancer treatment are
an iatrogenic effect; given that we have
caused the problem, do we not have
some obligation to address it? Secondly,
while there are experts to refer peo-
ple to in some communities, these are
not plentiful and, indeed, are exception-
ally scarce in some communities. Where
they do exist, the services can be expen-
sive. Further, some of my private practice
colleagues tell me they are not well pre-
pared to address sexual aspects of can-
cer. Furthermore, most of the problems
(in the vicinity of 80% according to one
study by Schover) do not require the ser-
vices of a sex therapist, but can be well
addressed through education and coach-
ing by HCPs who have some training in
the area. I think we have an obligation to
recognize the issues and do something to
address them.
Things are changing in Canada
though. Psychosocial distress screen-
ing has become a priority focus for prac-
tice change in many centres, and sexual
health seems to be getting a lot of atten-
tion, judging by the interest in courses
like IPODE’s Sexual Health Counselling
in Cancer courses and commitments by
agencies to purchase bulk discounts for
their staff. Sexual health is no longer seen
as everyone’s and no one’s responsibility.
Rather, more and more nurses are finding
ways to ask about concerns in this area
and to address or refer people who need
help.
Not all the concerns are about sex-
uality, of course; there are a myriad of
serious effects of treatments such as
androgen deprivation therapy (ADT), for
example, and few standardized programs
for helping men and partners to address
these. The distress men experience while
on ADT can be, perhaps often is, pro-
found. Body feminization, shrinking geni-
tals and loss of libido and sexual function
have an effect on how men experience
being a man, whether or not they wished
to be, or were sexually active. There are
many physical effects such as increased
cardiovascular risk that are obviously
important, too.
In this issue, we have three articles
addressing various aspects of pros-
tate cancer and an editorial by Richard
Wassersug, a prostate cancer patient,
scientist and lead author on the new
book Androgen Deprivation Therapy:
An Essential Guide for Prostate Cancer
Patients and Their Partners (www.
lifeonADT.com). Wassersug, humor-
ously and frankly, highlights for us
some of the “hits” and “misses” in his
interactions with nurses during his care.
We hope our readers find the articles
both interesting and useful in informing
their practice.
Deborah McLeod,
Guest Editor
Guest Editorial
Deborah L. McLeod, Dalhousie University, School of Nursing and Capital Health/QEII
Cancer Care Program, Halifax, Nova Scotia, Canada
 6
6
 7
7
 8
8
 9
9
 10
10
 11
11
 12
12
 13
13
 14
14
 15
15
 16
16
 17
17
 18
18
 19
19
 20
20
 21
21
 22
22
 23
23
 24
24
 25
25
 26
26
 27
27
 28
28
 29
29
 30
30
 31
31
 32
32
 33
33
 34
34
 35
35
 36
36
 37
37
 38
38
 39
39
 40
40
 41
41
 42
42
 43
43
 44
44
 45
45
 46
46
 47
47
 48
48
 49
49
 50
50
 51
51
 52
52
 53
53
 54
54
 55
55
 56
56
 57
57
 58
58
 59
59
 60
60
 61
61
 62
62
 63
63
 64
64
 65
65
 66
66
 67
67
 68
68
 69
69
 70
70
 71
71
 72
72
 73
73
 74
74
 75
75
 76
76
 77
77
 78
78
 79
79
 80
80
 81
81
 82
82
 83
83
 84
84
 85
85
 86
86
 87
87
 88
88
 89
89
 90
90
 91
91
 92
92
 93
93
 94
94
 95
95
 96
96
 97
97
 98
98
 99
99
 100
100
 101
101
 102
102
 103
103
 104
104
 105
105
 106
106
 107
107
 108
108
1
/
108
100%