NUTRICASUS NUTRICASUS

Editorial
L‘alimentation. Une arme efficace pour nos enfants face à l'agression microbienne de la sphère ORL
Les cartables sentent bon le neuf, les cahiers sont fraîchement recouverts. Les arômes de l'automne se font de
plus en plus présents. C’est le moment de la résurgence des infections des voies respiratoires. La période du
retour des atteintes ORL qui, chez certains enfants, deviennent trop souvent récidivantes. Ces affections
accroissent considérablement la fréquence des consultations médicales, des prescriptions médicamenteuses, des
jours d’absentéisme scolaire ou d’arrêt de travail, et génèrent d’importants coûts induits. Les rhinopharyngites
représentent un réel problème de santé publique.Le plus souvent d'origine virale, elles n’en sont pas moins une
des toutes premières causes de prescription d’antibiotiques chez l’enfant. Dans près de 40% des cas de
rhinopharyngite, un antibiotique est administré alors qu’aucune étude n‘en a jamais démontré l'efficacité dans cette
affection, ni en terme de durée de la maladie, ni dans la prévention de ses complications. La médecine
nutritionnelle offre une réelle opportunité d'augmenter de manière saine la résistance de l'enfant aux agresseurs
microbiens. Elle crée les conditions optimales pour exprimer une réponse immunitaire adaptée et efficace en
équilibrant le statut en zinc, cuivre, sélénium et fer, en optimalisant le ratio des acides gras oméga-3/oméga-6, et
en restaurant une flore intestinale eubiotique. L'immunisation contre des antigènes alimentaires (en particulier les
protéines du lait et de l'œuf mais aussi le gluten et le froment) peut perturber le travail du système immunitaire et
fragiliser l'individu face aux agents microbiens. Un bilan de base visualise le statut nutritionnel de l'enfant (ou de
l'adulte) et permet de personnaliser la correction des carences et excès afin de garantir les conditions d’une
réponse immune optimale et ….d’une rentrée sans soucis.
Nutritionnellement vôtre,
Ellipsys S.A.
Editorial
L‘alimentation. Une arme efficace pour nos enfants face à l'agression microbienne de la sphère ORL
Les cartables sentent bon le neuf, les cahiers sont fraîchement recouverts. Les arômes de l'automne se font de
plus en plus présents. C’est le moment de la résurgence des infections des voies respiratoires. La période du
retour des atteintes ORL qui, chez certains enfants, deviennent trop souvent récidivantes. Ces affections
accroissent considérablement la fréquence des consultations médicales, des prescriptions médicamenteuses, des
jours d’absentéisme scolaire ou d’arrêt de travail, et génèrent d’importants coûts induits. Les rhinopharyngites
représentent un réel problème de santé publique.Le plus souvent d'origine virale, elles n’en sont pas moins une
des toutes premières causes de prescription d’antibiotiques chez l’enfant. Dans près de 40% des cas de
rhinopharyngite, un antibiotique est administré alors qu’aucune étude n‘en a jamais démontré l'efficacité dans cette
affection, ni en terme de durée de la maladie, ni dans la prévention de ses complications. La médecine
nutritionnelle offre une réelle opportunité d'augmenter de manière saine la résistance de l'enfant aux agresseurs
microbiens. Elle crée les conditions optimales pour exprimer une réponse immunitaire adaptée et efficace en
équilibrant le statut en zinc, cuivre, sélénium et fer, en optimalisant le ratio des acides gras oméga-3/oméga-6, et
en restaurant une flore intestinale eubiotique. L'immunisation contre des antigènes alimentaires (en particulier les
protéines du lait et de l'œuf mais aussi le gluten et le froment) peut perturber le travail du système immunitaire et
fragiliser l'individu face aux agents microbiens. Un bilan de base visualise le statut nutritionnel de l'enfant (ou de
l'adulte) et permet de personnaliser la correction des carences et excès afin de garantir les conditions d’une
réponse immune optimale et ….d’une rentrée sans soucis.
Nutritionnellement vôtre,
Ellipsys S.A.
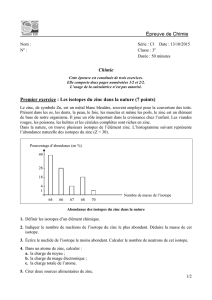
Le Cas Clinique du mois : Enfant de six ans, rhinopharyngites récidivantes
Histoire du Patient
Motif de la consultation :
Enfant de six ans amené à la consultation de médecine nutritionnelle pour des
rhinopharyngites à répétition, compliquées de bronchites asthmatiformes, au moins
trois à quatre fois par cycle automne/hiver et ce, depuis l'âge de trois ans (entrée à
l'école). L'année précédente, l'enfant a été pendant quatre mois sous antibiotiques.
Anamnèse :
• Petit garçon de six ans et demi.
• Deuxième enfant d'une famille de trois (une sœur de 9 ans et un frère de 3 ans).
• Parents en bonne santé.
• Père fumeur (aussi en présence des enfants).
• Les frère et sœur du jeune patient souffrent également de rhinopharyngites mais
moins fréquentes et surtout complications bronchitiques.
Clinique
• Poids : 18 kilos ; Taille : 115 cm.
• Enfant maigre et pâle, ongles striés, langue chargée.
• Nez encombré.
Examens de Biologie Fonctionnelle et Nutritionnelle prescrits :
• Profil des acides gras.
• Etat des défenses anti-oxydantes (notamment zinc) et marqueurs de stress oxydant.
• IgG alimentaires.
Histoire du Patient
Motif de la consultation :
Enfant de six ans amené à la consultation de médecine nutritionnelle pour des
rhinopharyngites à répétition, compliquées de bronchites asthmatiformes, au moins
trois à quatre fois par cycle automne/hiver et ce, depuis l'âge de trois ans (entrée à
l'école). L'année précédente, l'enfant a été pendant quatre mois sous antibiotiques.
Anamnèse :
• Petit garçon de six ans et demi.
• Deuxième enfant d'une famille de trois (une sœur de 9 ans et un frère de 3 ans).
• Parents en bonne santé.
• Père fumeur (aussi en présence des enfants).
• Les frère et sœur du jeune patient souffrent également de rhinopharyngites mais
moins fréquentes et surtout complications bronchitiques.
Clinique
• Poids : 18 kilos ; Taille : 115 cm.
• Enfant maigre et pâle, ongles striés, langue chargée.
• Nez encombré.
Examens de Biologie Fonctionnelle et Nutritionnelle prescrits :
• Profil des acides gras.
• Etat des défenses anti-oxydantes (notamment zinc) et marqueurs de stress oxydant.
• IgG alimentaires.
NUTRICASUS
Le Journal de la Médecine Nutritionnelle et Fonctionnelle Pratique
N7, septembre 2006
NUTRICASUS
Le Journal de la Médecine Nutritionnelle et Fonctionnelle Pratique
N7, septembre 2006

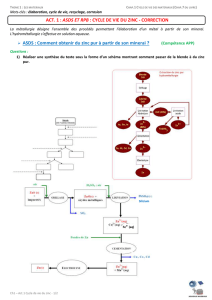
Le Cas Clinique du Mois : Résultats et Interprétation
Le bilan nutritionnel de cet enfant de 6 ans est perturbé et explique en grande partie sa vulnérabilité immunitaire,
responsable de ses rhinopharyngites récidivantes avec complications. Le taux en zinc est largement insuffisant. Cofacteur
indispensable au fonctionnement efficace des barrières respiratoires, le zinc intervient dans le fonctionnement du thymus
et conditionne l’efficacité de la réponse immunitaire adaptative. Cette carence en zinc et la déficience en vitamine A y
associée expliquent l’état de stress oxydant dont souffre le patient. Une alimentation très pauvre en fruits et légumes
contribue à la fragilité de ses cellules face aux radicaux libres. L'enfant est carencé en acides gras oméga-3, tant au
niveau du précurseur (LNA) que de ses dérivés allongés (EPA, DHA). Face à une agression microbienne, la réaction
inflammatoire sera démesurée et les manifestations cliniques importantes. Les lymphocytes Th2 stimuleront la production
d'IgE. Enfin, la présence d'IgG dirigées contre les protéines du lait et de l’œuf signent une digestion incomplète de ces
protéines et une altération de la fonction «barrière» qu’assume la muqueuse intestinale. Ces IgG peuvent entretenir une
réaction inflammatoire au niveau de l'intestin, altérant ainsi l’efficacité de l’important système immunitaire qu’il abrite. Sont
hautement recommandées, une supplémentation en zinc et huile de poisson, une correction alimentaire et la suppression
de la consommation de lait et d'œuf, ou à tout le moins, une diminution de la fréquence et de la quantité d’ingestion des
lait et œufs, sans oublier les aliments qui en contiennent.
Le bilan nutritionnel de cet enfant de 6 ans est perturbé et explique en grande partie sa vulnérabilité immunitaire,
responsable de ses rhinopharyngites récidivantes avec complications. Le taux en zinc est largement insuffisant. Cofacteur
indispensable au fonctionnement efficace des barrières respiratoires, le zinc intervient dans le fonctionnement du thymus
et conditionne l’efficacité de la réponse immunitaire adaptative. Cette carence en zinc et la déficience en vitamine A y
associée expliquent l’état de stress oxydant dont souffre le patient. Une alimentation très pauvre en fruits et légumes
contribue à la fragilité de ses cellules face aux radicaux libres. L'enfant est carencé en acides gras oméga-3, tant au
niveau du précurseur (LNA) que de ses dérivés allongés (EPA, DHA). Face à une agression microbienne, la réaction
inflammatoire sera démesurée et les manifestations cliniques importantes. Les lymphocytes Th2 stimuleront la production
d'IgE. Enfin, la présence d'IgG dirigées contre les protéines du lait et de l’œuf signent une digestion incomplète de ces
protéines et une altération de la fonction «barrière» qu’assume la muqueuse intestinale. Ces IgG peuvent entretenir une
réaction inflammatoire au niveau de l'intestin, altérant ainsi l’efficacité de l’important système immunitaire qu’il abrite. Sont
hautement recommandées, une supplémentation en zinc et huile de poisson, une correction alimentaire et la suppression
de la consommation de lait et d'œuf, ou à tout le moins, une diminution de la fréquence et de la quantité d’ingestion des
lait et œufs, sans oublier les aliments qui en contiennent.
NUTRICASUS
Le Journal de la Médecine Nutritionnelle et Fonctionnelle Pratique
NUTRICASUS
Le Journal de la Médecine Nutritionnelle et Fonctionnelle Pratique
• Carence en acides gras oméga-3: elle touche
le précurseur acide alpha-linolénique (LNA),
et ses dérivés allongés acide eïcosapentaénoïque
(EPA), et acide docosahexanénoïque (DHA).
• La delta-6-désaturase fonctionne relativement bien
• Rapport AA/EPA largement en faveur de l'acide
arachidonique, situation qui favorise grandement
les réactions inflammatoires exagérées et la
production d'IgE (stimulation de la réponse Th2).
• Carence en acides gras oméga-3: elle touche
le précurseur acide alpha-linolénique (LNA),
et ses dérivés allongés acide eïcosapentaénoïque
(EPA), et acide docosahexanénoïque (DHA).
• La delta-6-désaturase fonctionne relativement bien
• Rapport AA/EPA largement en faveur de l'acide
arachidonique, situation qui favorise grandement
les réactions inflammatoires exagérées et la
production d'IgE (stimulation de la réponse Th2).
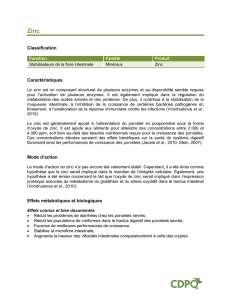
• Stress oxydant avec taux anormalement élevé de la
8-hydroxyguanosine.
• Subcarence en vitamine A.
• Carence importante en zinc.
• Taux de sélénium trop élevé.
• Taux de cuivre modérément augmenté.
• Stress oxydant avec taux anormalement élevé de la
8-hydroxyguanosine.
• Subcarence en vitamine A.
• Carence importante en zinc.
• Taux de sélénium trop élevé.
• Taux de cuivre modérément augmenté.
IgG ALIMENTAIRES
Taux d'IgG anormalement élevé pour les protéines
du lait et de l’œuf. Pas de taux anormaux d’IgG
contre le gluten, le froment et autres céréales.
Taux d'IgG anormalement élevé pour les protéines
du lait et de l’œuf. Pas de taux anormaux d’IgG
contre le gluten, le froment et autres céréales.
PROFIL DES ACIDES GRAS
PROFIL DEFENSES ANTI-OXYDANTES ET STRESS OXYDATIF

Nutrition et Immunités : Références Scientifiques Choisies
NUTRICASUS
Le Journal de la Médecine Nutritionnelle et Fonctionnelle Pratique
NUTRICASUS
Le Journal de la Médecine Nutritionnelle et Fonctionnelle Pratique
An open-label, single-center, phase IV clinical study of the effectiveness of
zinc gluconate glycine lozenges (Cold-Eeze) in reducing the duration and
symptoms of the common cold in school-aged subjects. McElroy
BH, Miller SP. Am J Ther. 2003 Sep-Oct;10(5):324-9.
Each year, more than 62 million cases of the common cold in the United States
require medical attention and more than 80% affect school-aged children. The
objective of this prospective, intent-to-treat, phase IV study was to determine
the therapeutic and prophylactic effectiveness of zinc gluconate glycine
lozenges (Cold-Eeze) for the common cold. Zinc lozenges were administered
once daily during the cold season for prophylaxis. For therapeutic purposes,
lozenges were given 4 times per day. The primary objective of the study was
the treatment effect on cold duration, and the secondary objective was the effect
on the number of common colds. A putative control from our previous study
was used for comparison. A total of 178 children, ages 12 to 18 years, was
enrolled, of which 134 met criteria for efficacy analysis. The average cold
duration with therapeutic lozenge use was 6.9 +/- 3.1 days, significantly shorter
than the 9.0 +/- 3.5 days found in the control group (P < 0.001). The mean
number of colds was 1.28 +/- 1.03 with zinc lozenge prophylaxis versus 1.7 +/-
1.91 without prophylaxis (P < 0.05), a 25% reduction. With prophylaxis, 25%
of the subjects did not experience a cold and two-thirds never had a cold or only
had 1 cold. There was no antibiotic use for any cold, and there were no adverse
events reported. Results of this study are consistent with those from our
previous retrospective study showing significantly shorter cold duration and
fewer colds with the use of zinc gluconate glycine lozenges. The zinc gluconate
glycine lozenges are well tolerated and are an easy-to-administer therapy that
has the potential to substantially reduce cold-related school absences and
antibiotic use and misuse as well as to provide a cost saving.
Essential fatty acids: the effects of dietary supplementation among children
with recurrent respiratory infections. Venuta
A, Spano C, Laudizi L, Bettelli F, Beverelli A, Turchetto E. J Int
Med Res. 1996 Jul-Aug;24(4):325-30. The impact of dietary supplementation with
essential fatty acids (EFA) on recurrent respiratory infections (RRI) in children was
evaluated by means of a randomized cross-over double-blind study. Linoleic acid
(596 mg/day) and alpha-linolenic acid [855 mg/day] as a commercial preparation or
placebo (olive oil) were administered for two consecutive winter seasons
(November to February, T0-T120) to 20 children affected by RRI, aged between 36
and 49 months. Plasma levels of n-3 and n-6 metabolites increased after the
administration of EFA. The number of infective episodes, days' fever and days'
absence from school were reduced significantly during the observation period
(extended from T120 to T180) in children receiving EFA supplementation. Our
results suggest that n-3 and n-6 polyunsaturated fatty acids may play a favourable
role in the defence mechanism of these subjects.
Plusieurs milliers de publications démontrent que
les défenses innées et adaptatives voient l’efficacité
et la mesure de leurs réponses optimalisées par un
bon équilibre alimentaire. L’importance du zinc et des
acides gras oméga-3 appartient désormais à la
médecine basée sur l'évidence (EBM). L'intégrité
fonctionnelle du tube digestif est également une
condition déterminante pour que notre système
immunitaire fonctionne correctement.
Nutrition and the immune system from birth to old age.
Chandra RK.
Eur J Clin Nutr 2002 Aug;56 Suppl 3:S73-6
For millennia, food has been at the center of social events, in times of joy and in
times of sorrow. Protein-energy malnutrition is associated with a significant
impairment of cell-mediated immunity, phagocyte function, complement system,
secretory immunoglobulin A antibody concentrations, and cytokine production.
Deficiency of single nutrients also results in altered immune response: this is
observed even when the deficiency state is relatively mild. Of the micronutrients,
zinc, selenium, iron, copper, vitamins A, C, E and B(6), and folic acid have
important influences on immune responses. Overnutrition and obesity also reduce
immunity. Low-birth-weight infants have a prolonged impairment of cell-mediated
immunity that can be partly restored by providing extra amounts of dietary zinc. In
the elderly, impaired immunity can be enhanced by modest amounts of a
combination of micronutrients. These findings have considerable practical and
public health significance.
Zinc supplementation reduces the incidence of acute lower respiratory
infections in infants and preschool children: a double-blind, controlled
trial. Sazawal
S, Black RE, Jalla S, Mazumdar S, Sinha A, Bhan MK. Pediatrics. 1998
Jul;102(1 Pt 1):1-5.
BACKGROUND: Increased acute lower respiratory infection incidence,
severity, and mortality are associated with malnutrition, and reduced
immunological competence may be a mechanism for this association. Because
zinc deficiency results in impaired immunocompetence and zinc
supplementation improves immune status, we hypothesized that zinc deficiency
is associated with increased incidence and severity of acute lower respiratory
infection. METHODS: We evaluated the effect of daily supplementation with
10 mg of elemental zinc on the incidence and prevalence of acute lower
respiratory infection in a double-blind, randomized, controlled trial in 609
children (zinc, n = 298; control, n = 311) 6 to 35 months of age.
Supplementation and morbidity surveillance were done for 6 months.
RESULTS: After 120 days of supplementation, the percentage of children with
plasma zinc concentrations <60 microg/dL decreased from 35.6% to 11.6% in
the zinc group, whereas in the control group it increased from 36.8% to 43.6%.
Zinc-supplemented children had 0.19 acute lower respiratory infection
episodes/child/year compared with 0.35 episodes/child/year in the control
children. After correction for correlation of data using generalized estimating
equation regression methods, there was a reduction of 45% (95% confidence
interval, 10% to 67%) in the incidence of acute lower respiratory infections in
zinc-supplemented children. CONCLUSIONS: A dietary zinc supplement
resulted in a significant reduction in respiratory morbidity in preschool children.
These findings suggest that interventions to improve zinc intake will improve
the health and survival of children in developing countries.
Tight junctions, leaky intestines, and pediatric diseases.
Liu Z, Li N, Neu J.
Acta Paediatr. 2005 Apr;94(4):386-93.
BACKGROUND: Tight junctions (TJs) represent the major barrier within the
paracellular pathway between intestinal epithelial cells. Disruption of TJs leads to
intestinal hyperpermeability (the so-called "leaky gut") and is implicated in the
pathogenesis of several acute and chronic pediatric disease entities that are likely to
have their origin during infancy. AIM: This review provides an overview of
evidence for the role of TJ breakdown in diseases such as systemic inflammatory
response syndrome (SIRS), inflammatory bowel disease, type 1 diabetes, allergies,
asthma, and autism. CONCLUSION: A better basic understanding of this structure
might lead to prevention or treatment of these diseases using nutritional or other
means.
Ingested probiotics reduce nasal colonization with pathogenic bacteria
(Staphylococcus aureus, Streptococcus pneumoniae, and beta-hemolytic
streptococci).
Gluck U, Gebbers JO.
Am J Clin Nutr 2003 Feb;77(2):517-20
BACKGROUND: As a bacterial reservoir, the nose may harbor potentially
pathogenic bacteria (PPB: Staphylococcus aureus, Streptococcus pneumoniae, beta-
hemolytic streptococci, and Haemophilus influenzae). In patients carrying PPB,
antiseptic regimens could be crucial for infection control after major operations on or
injuries of the head, nasal sinuses, or lungs. Such regimens may also be important
for diabetic patients and persons receiving hemodialysis, in intensive care units, or
with impaired immunity due to various other causes. OBJECTIVE: We tested a
possible effect of the ingestion of probiotics on the bacterial flora of the nose.
DESIGN: In an open, prospective trial, 209 volunteers were randomly assigned to
consume either a probiotic, fermented milk drink [65 mL with Lactobacillus GG
(ATCC 53103), Bifidobacterium sp B420, Lactobacillus acidophilus 145, and
Streptococcus thermophilus; n = 108] or standard yogurt (180 g; n = 101) daily for 3
wk. Nasal microbial flora were analyzed on days 1, 21, and 28. The microbial
examination was blinded to the source of the samples. RESULTS: We found a
significant reduction (19%; P < 0.001) in the occurrence of nasal PPB in the group
who consumed the probiotic drink but not in the group who consumed yogurt. The
effect was mainly on gram-positive bacteria, which decreased significantly (P <
0.05). CONCLUSIONS: The results indicate that regular intake of probiotics can
reduce PPB in the upper respiratory tract. The results also indicate a linkage of the
lymphoid tissue between the gut and the upper respiratory tract.

CLINIQUE ET LABORATOIRE, UNE SYNERGIE INDISPENSABLE.
CLINIQUE ET LABORATOIRE, UNE SYNERGIE INDISPENSABLE.
SUR LE PLAN PRATIQUE.
SUR LE PLAN PRATIQUE.
Editeur responsable
Ellipsys S.A.
Green Alley Office Park
70 Rue du Panier Vert
B-1400 Nivelles
Belgique Nutricasus est rédigé par des experts dans le domaine de la nutrition
info@ellipsys.be sous la supervision du comité scientifique du laboratoire Roman Païs.
Editeur responsable
Ellipsys S.A.
Green Alley Office Park
70 Rue du Panier Vert
B-1400 Nivelles
Belgique Nutricasus est rédigé par des experts dans le domaine de la nutrition
info@ellipsys.be sous la supervision du comité scientifique du laboratoire Roman Païs.
NUTRICASUS
Le Journal de la Médecine Nutritionnelle et Fonctionnelle Pratique
NUTRICASUS
Le Journal de la Médecine Nutritionnelle et Fonctionnelle Pratique
Arthrite rhumatoïde et alimentation : Réalité ou fantaisie ?
Août 2006. Oslo. Des patients, souffrant d’arthrite rhumatoïde, signalent régulièrement que les crises
douloureuses sont plus intenses après l’absorption de certains aliments. « Psychosomatique » ??
Le Dr Per Brandtzaeg et son équipe vont tenter de savoir si des aliments peuvent intensifier des réactions
inflammatoires. Ils interrogent les patients pour identifier les éventuels aliments à l’origine de ces
phénomènes inflammatoires. Mais surtout, ils prélèvent du sang et du liquide du système lymphatique
intestinal chez les volontaires. Et là, le doute n’est plus permis. Les taux d’anticorps sont élevés, et
particulièrement contre des composants du lait, des œufs, du porc et des poissons.
L’étude est certes plus complexe que cette brève évocation. Mais elle prouve, si
tant est besoin, qu’une anamnèse bien conduite est essentielle. Si votre patient
(polyarthritique, ou autre) vous dit souffrir plus quand il consomme certains
aliments, écoutez-le et questionnez-le. Dites-lui qu’il existe bel et bien une
explication et pensez à notre petit patient. Tentez d’objectiver ses plaintes par les
IgG et conseillez-lui d’éviter au maximum les produits contenant le (ou les)
aliment(s) qui lui rend(ent) la vie très inconfortable. (Gut, 2006;55:1240)
L’apport du dosage sérique des IgG « alimentaires ».
Les dosages des IgG et IgE sanguines sont réalisés par un test récent, portant le label de «troisième
génération» et reconnu par la FDA (USA). Facilement automatisable, la méthode est quantitative et les
dosages sont effectués dans des conditions de reproductibilité permettant une bonne fiabilité.
L’allergie, au sens où nous l’entendons habituellement, est une réaction de type 1 généralement aiguë et
médiée par les IgE. Le patient identifie rapidement l’élément déclenchant et le diagnostic peut
généralement être confirmé par des taux perturbés d’IgE spécifiques.
Notre petit patient présente des taux élevés d’IgG. Il s’agit donc d’un autre type de réaction immune.
Dans le syndrome du colon irritable, Atkinson (Gut, 2004;53:1459) a démontré que la diminution des
manifestations cliniques était nettement plus marquée chez les patients suivant un régime d’éviction
spécifique basé sur les valeurs des IgG sériques plutôt qu’un régime d’exclusion standard.
Le dosage des IgG et IgE spécifiques se pratique sur sérum (tube rouge).
Ces analyses consomment relativement peu de sérum et un tube de sang
en plus des quantités habituelles suffit amplement.
Les IgG et IgE sont stables et supportent bien le transport. Il est néanmoins
recommandé d’acheminer les prélèvements rapidement afin d’éviter
l’hémolyse.
1
/
4
100%