Perinatal Mental Health Teams & Outcomes in Pregnant Women: England Study
Telechargé par
ghivi15

174
www.thelancet.com/psychiatry Vol 11 March 2024
Articles
Community perinatal mental health teams and associations
with perinatal mental health and obstetric and neonatal
outcomes in pregnant women with a history of secondary
mental health care in England: a national population-based
cohort study
Ipek Gurol-Urganci*, Julia Langham*, Emma Tassie, Margaret Heslin, Sarah Byford, Antoinette Davey, Helen Sharp, Dharmintra Pasupathy,
Jan van der Meulen†, Louise M Howard†, Heather A O’Mahen†
Summary
Background Women with a pre-existing severe mental disorder have an increased risk of relapse after giving birth. We
aimed to evaluate associations of the gradual regional implementation of community perinatal mental health teams
in England from April, 2016, with access to mental health care and with mental health, obstetric, and neonatal
outcomes.
Methods For this cohort study, we used the national dataset of secondary mental health care provided by National Health
Service England, including mental health-care episodes from April 1, 2006, to March 31, 2019, linked at patient level to
the Hospital Episode Statistics, and birth notifications from the Personal Demographic Service. We included women
(aged ≥18 years) with an onset of pregnancy from April 1, 2016, who had given birth to a singleton baby up to
March 31, 2018, and who had a pre-existing mental disorder, defined as contacts with secondary mental health care in the
10 years immediately before pregnancy. The primary outcome was acute relapse, defined as psychiatric hospital admission
or crisis resolution team contact in the postnatal period (first year after birth). Secondary outcomes included any
secondary mental health care in the perinatal period (pregnancy and postnatal period) and obstetric and neonatal
outcomes. Outcomes were compared according to whether a community perinatal mental health team was available
before pregnancy, with odds ratios (ORs) adjusted for time trends and maternal characteristics (adjORs).
Findings Of 807 798 maternity episodes in England, we identified 780 026 eligible women with a singleton birth, of
whom 70 323 (9·0%) had a pre-existing mental disorder. A postnatal acute relapse was found in 1117 (3·6%) of
31 276 women where a community perinatal mental health team was available and in 1745 (4·5%) of 39 047 women
where one was unavailable (adjOR 0·77, 95% CI 0·64–0·92; p=0·0038). Perinatal access to any secondary mental
health care was found in 9888 (31·6%) of 31 276 women where a community perinatal mental health team was
available and 10 033 (25·7%) of 39 047 women where one was not (adjOR 1·35, 95% CI 1·23–1·49; p<0·0001). Risk of
stillbirth and neonatal death was higher where a community perinatal mental health team was available (165 [0·5%]
of 30 980 women) than where it was not (151 [0·4%] of 38 693 women; adjOR 1·34, 95% CI 1·09–1·66; p=0·0063), as
was the risk of a baby small for gestational age (2227 [7·2%] of 31 030 women vs 2542 [6·6%] of 38 762 women;
adjOR 1·10, 1·02–1·20; p=0·016), whereas preterm birth risk was lower (3167 [10·1%] of 31 206 women vs 4341 [11·1%]
of 38 961; adjOR 0·86, 0·74–0·99; p=0·032).
Interpretation The regional availability of community perinatal mental health teams reduced the postnatal risk of
acute relapse and increased the overall use of secondary mental health care. Community perinatal mental health
teams should have close links with maternity services to avoid intensive psychiatric support overshadowing obstetric
and neonatal risks.
Funding The National Institute for Health and Care Research.
Copyright © 2024 The Author(s). Published by Elsevier Ltd. This is an Open Access article under the CC BY 4.0 license.
Introduction
Women with a pre-existing mental disorder are at
increased risk of a recurrence or exacerbation of their
mental health problems during the perinatal period.1
For example, a 2016 systematic review2 showed women
with pre-existing bipolar disorder had more than
20% risk of relapse in the postnatal period. A previous
study3 that we carried out in England, which included
all women giving birth between 2014 and 2018, also
showed an increased risk of adverse obstetric, neonatal,
and maternal outcomes in women who had a
pre-pregnancy secondary mental health-care contact,
Lancet Psychiatry 2024;
11: 174–82
Published Online
January 23, 2024
https://doi.org/10.1016/
S2215-0366(23)00409-1
*Joint first authors
†Joint senior authors
Department of Health Services
Research and Policy, London
School of Hygiene & Tropical
Medicine, London, UK
(I Gurol-Urganci PhD,
J Langham PhD,
Prof J van der Meulen PhD);
King’s Health Economics
(E Tassie MSc, M Heslin PhD,
Prof S Byford PhD) and Section
of Women’s Mental Health
(Prof L M Howard PhD),
Institute of Psychiatry,
Psychology and Neuroscience,
and Department of Women
and Children’s Health
(Prof D Pasupathy PhD), King’s
College London, London, UK;
Department of Primary Care
and Mental Health, University
of Liverpool, Liverpool, UK
(Prof H Sharp PhD);
Reproduction and Perinatal
Centre, Faculty of Medicine and
Health, University of Sydney,
Sydney, NSW, Australia
(Prof D Pasupathy); Washington
Singer Laboratories, University
of Exeter, Exeter, UK
(A Davey PhD,
Prof H A O’Mahen PhD)
Correspondence to:
Prof Jan van der Meulen,
Department of Health Services
Research and Policy, London
School of Hygiene & Tropical
Medicine, London WC1H 9SH,
UK
jan.vandermeulen@lshtm.
ac.uk

Articles
www.thelancet.com/psychiatry Vol 11 March 2024
175
with higher risks in women who had more recent
mental health-care contacts and in women who had a
contact that reflected a more severe mental health
disorder.
A guideline for the National Health Service (NHS) in
England, which was published in 2014, recommends that
women who have pre-existing complex and severe mental
illness should be referred to specialist mental health
services during pregnancy and the postnatal period,
preferably to a specialist community perinatal mental
health team for timely assessment and treatment.4,5 These
teams can counsel women planning a pregnancy and give
medication advice, oer psychological therapies, facilitate
bonding with the baby, and provide support for partners.6
Community perinatal mental health teams are also
expected to facilitate referral to the most appropriate
professionals in emergency situations. In 2016, NHS
England announced a 5-year investment of £365 million to
increase the overall availability of perinatal mental health
services, improve the treatment of women with new
mental health problems, and reduce the risk of relapse of
women with pre-existing mental disorders, particularly in
women at risk of severe acute relapses needing hospital
admission or the input of a mental health crisis resolution
team who provide intensive support in the community.7
The implementation initially prioritised areas that had
existing services that were not fully staed or areas that
already had robust service plans in place. Further
investment followed in 2019 with an aim to increase the
number of women for whom community perinatal
mental health teams are available during the perinatal
period and for pre-conception counselling.
We aimed to assess whether this gradual imple-
mentation of community perinatal mental health teams
was associated with an increase in the overall use of
secondary mental health-care services and a reduction
in the risk of acute relapse in the postnatal period.
Individuals are eligible to receive secondary mental
health care provided by NHS England if they have
complex, moderate, or severe mental health problems
that require a more intensive and specialist intervention
than primary care sta can provide. To access secondary
mental health care, patients typically need a referral from
a general practitioner or to be seen as part of urgent or
emergency psychiatric care.8 Because of the increased
obstetric and neonatal risk in women with at least
one pre-pregnancy contact with secondary mental
health-care services,3 we also evaluated associations of
this gradual implementation with the risk of adverse
obstetric and neonatal outcomes.
Research in context
Evidence before this study
There is little evidence on the effectiveness of different models
to deliver perinatal mental health care. Many countries do not
have mental health-care practitioners who are specifically
trained for delivering care during the perinatal period, and
delivery models vary widely. We searched MEDLINE from
inception to Aug 7, 2023, for evidence on the effectiveness of
specialist community perinatal mental care or equivalent
initiatives, using the following search terms (“perinatal” AND
[“mental disorders” OR “mental illness”] AND “community”
AND [“team” OR “centre” OR “center”]) without language
restrictions. We did not find any studies directly comparing
mental health or obstetric and neonatal outcomes in women
with pre-existing mental disorders who did or did not have
support from specialist perinatal mental health teams located
in the community. A UK study of 24 women with emotional
dysregulation in the perinatal period, published in 2018,
suggested that behavioural therapy delivered by a community
perinatal team could reduce stress. Another UK study of
32 women suggested that recommendations from a specialist
perinatal mental health service were followed around 80% of
the time. Qualitative research has found that women prefer the
tailored care available in specialist perinatal mental health
services compared with generic care.
Added value of this study
In England, specialist community perinatal mental health teams
were rolled out from 2016. This initiative, which is unique in the
world, aimed to improve access to specialist treatment for
women with perinatal mental health problems and improve
mental health outcomes. We found that where a community
perinatal mental health team was available, there was an
increase in access to secondary mental health care (a psychiatric
hospital admission, a crisis resolution team contact, or
community care) during pregnancy and in the first year after
birth and a decrease in the risk of an acute relapse
(a hospital admission or crisis resolution team contact) in the
first year after birth. However, we also found an increase in the
risk of stillbirth and neonatal death, and birth of a baby small for
gestational age where a community perinatal mental health
team was available, and a decrease in the risk of preterm birth.
Implications of all the available evidence
The improved access to mental health services and reduction in
acute postpartum relapse suggests that other countries could
consider developing such specialist community perinatal
mental health services. Further research on whether adverse
obstetric outcomes are associated with community perinatal
mental health teams is urgently needed. Based on our evidence,
however, specialist perinatal mental health-care practitioners
working in the community should ensure that they work closely
with other health and social care professionals to minimise the
risk that more intensive psychiatric support available in a region
negatively affects the midwifery and obstetric support that
women with severe mental disorders receive during pregnancy
and childbirth.

Articles
176
www.thelancet.com/psychiatry Vol 11 March 2024
Methods
Study design and participants
This cohort study used three consecutive versions of the
national dataset of secondary mental health care provided
by NHS England, which together included mental health-
care episodes from April 1, 2006, to March 31, 2019, linked
at patient level to Hospital Episode Statistics, which is the
administrative database of all care episodes in general
NHS hospitals,9,10 and birth notifications from the
Personal Demographic Service, which is the national
master database of all NHS patients in England
containing patient details such as name, address, date of
birth, and NHS number.11 Records of mental health-care
episodes between Dec 1, 2015, and March 31, 2016, were
not available for technical reasons.
Records from the Hospital Episode Statistics database
included patient demographics, admission dates, diag-
noses coded according to ICD-10, and procedures coded
according to OPCS Classification of Inter ventions and
Procedures version 4 (OPCS-4) codes (appendix pp 2, 4).12
Each record of a maternity episode in the Hospital
Episode Statistics database contains a set of additional
data fields, often referred to as the maternity tail, which
contain specific information, including birthweight,
gestational age, and mode of delivery.9 Birth records from
the Personal Demographic Service contained additional
information on stillbirth, gestational age, sex of the baby,
and birthweight, which was used if Hospital Episode
Statistics data were missing. Ethics approval was provided
by the NHS Health Research Authority (19/SW/0218) and
data were provided by the NHS Data Access Request
Service (DARS-NIC-376141-W5D3L-v0.9).
For this study, from Hospital Episode Statistics records
and Personal Demographic Service birth notifications, we
identified maternity episodes of all women eligible for
inclusion (aged ≥18 years) with a recorded gestation
(≥24 completed weeks) with an onset of pregnancy from
April 1, 2016, and a singleton birth up to March 31, 2018.
This inclusion period was chosen because it allowed us to
determine the mental health outcomes according to the
most recent version of the secondary mental health
services dataset for all included women (appendix p 2).
Women who had multiple births were excluded for
practical reasons; first, their number was small, and
second, including them would have made the statistical
analysis more complex because it cannot be assumed
that the outcomes of babies of a multiple birth are
independent observations. If there were multiple
maternity episodes for the same woman during the study
period, one maternity episode was selected using a
random number generator to be included in the study to
minimise selection bias and, again, to avoid the need to
use more complex statistical methods appropriate for the
analysis of non-independent outcomes.
To determine the onset of pregnancy, we subtracted the
gestational age at birth minus 2 weeks (or 38 weeks if
gestational age was not available) from the date of birth.
Women were included if they had a pre-existing mental
illness, defined as a contact with any form of secondary
mental health care, within a look-back period of 10 years
before the onset of pregnancy.8 This 10-year look-back
period was chosen on pragmatic grounds, because the
historical mental health services data were available from
April 1, 2006.
Procedures
We distinguished three levels of secondary mental health
care as a proxy for the severity of the mental disorder.
The first level (hospital admission) was an admission to a
psychiatric ward, including generic psychiatric wards,
mother–baby units, or secure wards. The second level
(crisis resolution team) was the involvement of a mental
health crisis resolution team providing intensive
treatment at home for an acute mental health crisis
otherwise needing hospital admission. The third level
(community care) was any other secondary mental
health-care contact, including day care and outpatient or
community-based care. More information can be found
in a previous paper.3
We did not use recorded diagnostic information to
distinguish the nature or severity of the women’s mental
illness because of the high rate of missingness of
diagnostic information, especially in records of the crisis
resolution team or community care. It has been widely
recognised that mental health diagnoses are often not or
incompletely recorded in administrative datasets of
mental health care.13
Information on the regional availability of community
perinatal mental health teams was collected at the level of
the Clinical Commissioning Groups.14 These groups
were NHS bodies responsible for the planning and
commissioning of health-care services for their local
area between April 1, 2013, and July 31, 2022. Initially,
211 Clinical Commissioning Groups were established
in 2013; this number decreased to 135 in 2020 because of
mergers between groups. In this study, we define the
regions according to the 207 Clinical Commissioning
Groups present in July, 2017, given that these reflect as
accurately as possible the situation for the women
included in our study. Typically, these regions cover areas
with a population of 250 000 people. We surveyed the
Clinical Commissioning Groups to determine the date of
community perinatal mental health team implementation
for each region, defined as the earliest date that at least a
dedicated psychiatrist, psychologist, and specialist nurse
were in place. We considered a community perinatal
mental health team to be available to women if the date
of implementation in their Clinical Commissioning
Group region was before the onset of pregnancy.
Outcomes
The primary mental health outcome was acute relapse
(psychiatric hospital admission or crisis resolution
team contact) in the postnatal period (the first year after
See Online for appendix

Articles
www.thelancet.com/psychiatry Vol 11 March 2024
177
birth). The secondary mental health outcome was any
secondary care contact, defined as at least one secondary
mental health-care contact during the perinatal
period (during pregnancy and the first year after
birth), also including a community mental health-care
contact.
The study also examined obstetric and neonatal
outcomes, which were stillbirth or neonatal death within
7 days of birth, preterm birth (birth before 37 completed
weeks of gestation), birth of a baby born small for
gestational age (birthweight less than the tenth centile
using the UK WHO gestationally corrected growth
charts),15 and two composite adverse outcome indicators
that capture neonatal and maternal morbidity. The
English Neonatal Adverse Outcome Indicator for
liveborn babies is derived from the presence of 15 ICD-10
diagnoses and seven OPCS-4 procedure codes present in
the babies’ Hospital Episode Statistics records before
inpatient discharge after birth (appendix p 4).16 The
English Maternal Morbidity Outcome Indicator is derived
from 17 ICD-10 diagnoses and nine OPCS-5 procedure
codes in Hospital Episode Statistics records of the
maternity episode (appendix p 4).17 For the purpose of
this study, acute psychosis was not included in the
English Maternal Morbidity Outcome Indicator because
mental illness is an inclusion criterion for this study.
Although maternal mortality data were available, we did
not include maternal mortality as an outcome in this
study because of the low statistical power.18
Statistical analysis
The statistical analysis was not specified in a pre-
published study protocol given that there is little
experience with the English national mental health
services datasets. However, the definitions of levels and
timing of secondary mental health care are the same as
those in a previous study by our team.3 All obstetric and
neonatal outcomes follow accepted definitions.
Hospital Episode Statistics records provided data on
maternal age, parity and previous caesarean section,
maternal ethnicity, pre-existing hypertension, pre-existing
diabetes, pre-eclampsia and eclampsia, and gestational
diabetes (appendix p 4). Socioeconomic deprivation was
derived from the quintiles of the national ranking of the
Index of Multiple Deprivation 2019 of the women’s area
of residence.19 The pre-pregnancy secondary mental
health-care contacts were grouped according to the
highest level of care received and according to the timing
of the most recent contact.
Odds ratios with risk adjustment (adjORs) and their
95% CI were estimated with logistic regression. Models
were fitted with robust standard errors to account for
clustering of outcomes within regions. We estimated
three models: model 1 provided the unadjusted estimates;
model 2 included adjustment for time trends (monthly,
assuming constant relative change in the outcome in
each subsequent month); and model 3 also included risk
Figure 1: Trial profile
*Numbers do not add up to total excluded due to episodes excluded for more than one criterion above.
31
276 women in regions with a community
perinatal mental health team available
at onset of pregnancy
70
323 women with a mental health-care
contact before pregnancy
709
703 excluded women without secondary mental
health-care contact in 10 years before pregnancy
39
047 women in regions without a
community perinatal mental health
team available at onset of pregnancy
780
026 eligible women with one maternity
episode
Of 5105 women with multiple maternity episodes,
one episode was chosen at random
785
131 eligible maternity episodes
807
798 maternity episodes in England,
with onset of pregnancy between
April 1, 2016, and March 31, 2018
22
667 excluded maternity episodes*
1665 residing in Wales, Northern Ireland, or
unknown residential region
5646 maternal age <18 years
14
323 multiple births
1312 gestational age <24 weeks
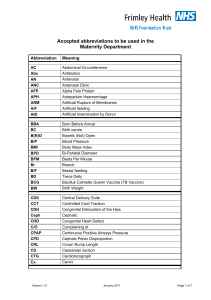
Figure 2: Regional availability of community perinatal mental health teams in 207 regions defined according
to regions covered by NHS Clinical Commissioning Groups between 2013 and 2019
Each horizontal bar represents a region.
June, 2013 June, 2014 June, 2015 June, 2016 June, 2017 June, 2018 June, 2019
0
20
40
60
80
100
120
140
160
180
200
No community perinatal mental health
team available
Community perinatal mental health
team available
Number of community perinatal mental health teams
Calendar time (month, year)

Articles
178
www.thelancet.com/psychiatry Vol 11 March 2024
adjustment for all maternal characteristics defined above
and the level and timing of pre-pregnancy secondary
mental health-care contacts.
In response to results of the analysis of obstetric and
neonatal adverse outcomes in women with pre-existing
mental disorders, we used the same methods to
compare these outcomes according to whether a
community perinatal mental health team was available
in women without a pre-existing mental disorder
(ie, without a secondary mental health-care contact in
the 10 years before pregnancy). We also carried out two
sub-group analyses: the first included only women who
had a pre-pregnancy psychiatric hospital admission or
crisis resolution team contact, and the second included
women who had any secondary mental health-care
contact in the year immediately before the pregnancy.
Data were missing on perinatal mortality for maternal
records with missing mortality records for the babies (650
[0·9%] of 70 323), on small for gestational age for maternal
records with incomplete information on birthweight, sex
of the baby, or gestational age (531 [0·8%] of 70 323), on
preterm births for maternal records with incomplete
information on gestational age (0·2% [150 of 70 323]), and
on neonatal and maternal adverse outcomes for unlinked
maternal records (2·6% [1797 of 70 096]) or those
identified from Personal Demographic Service records
only (5·1% [3589 of 70 323]). For all regression analyses,
missing outcomes and risk factors were imputed using
chained equations generating ten datasets with estimates
across imputed datasets pooled using Rubin’s rules.20
Stata (version 17) was used for all analyses. A p value of
less than 0·05 was considered to represent statistical
significance.
Role of the funding source
The funder had no role in study design, data collection,
data analysis, data interpretation, or writing of the report.
Results
Of 807 798 maternity episodes in England with an onset
of pregnancy after April 1, 2016, and a birth before
April 1, 2018, we identified 780 026 eligible women with a
singleton birth, of whom 70 323 (9·0%) had a pre-existing
mental disorder (figure 1).
Figure 2 shows that in April, 2016, the first month of
our cohort, a community perinatal mental health team
was available in 81 (39%) of 207 Clinical Commissioning
Group regions. The number of regions with a
community perinatal mental health team increased to
130 (63%) of 207 Clinical Commissioning Group regions
in June, 2017, just before the onset of pregnancy of
women who gave birth in March, 2018. Of 70 323 included
women, 31 276 (44·5%) gave birth where a community
perinatal mental health team was available in their
region at the onset of pregnancy and 39 047 (55·5%) gave
birth where one was not available. The characteristics of
women with and without a community perinatal mental
health team available were broadly similar (table 1), with
a lower proportion of White women in regions with a
community perinatal mental health team than in regions
without.
Of the 70 323 included women, 2862 4·1% had an
acute relapse in the postnatal period (table 2). The risk of
acute relapse varied according to regional community
perinatal mental health team availability; of 31 276 women
who gave birth in a region where a community perinatal
All women
(N=70 323)
No community perinatal
mental health team at
onset of pregnancy
(n=39 047)
Community perinatal
mental health team at
onset of pregnancy
(n=31 276)
Maternal age, years*
18–24 17 463 (24·8%) 9971 (25·5%) 7492 (24·0%)
25–34 40 031 (56·9%) 22 219 (56·9%) 17 812 (57·0%)
35–39 10 216 (14·5%) 5489 (14·1%) 4727 (15·1%)
≥40 2607 (3·7%) 1364 (3·5%) 1243 (4·0%)
Obstetric history†
Nulliparous 22 665 (32·2%) 12 749 (32·7%) 9916 (31·7%)
Multiparous, no previous
caesarean section
35 423 (50·4%) 19 558 (50·1%) 15 865 (50·7%)
Multiparous, with previous
caesarean section
8646 (12·3%) 4700 (12·0%) 3946 (12·6%)
Ethnicity‡
White 54 965 (78·2%) 31 199 (79·9%) 23 766 (76·0%)
South Asian 3244 (4·6%) 1622 (4·2%) 1622 (5·2%)
Black 1779 (2·5%) 692 (1·8%) 1087 (3·5%)
Mixed 1332 (1·9%) 661 (1·7%) 671 (2·1%)
Other stated 1160 (1·6%) 525 (1·3%) 635 (2·0%)
Socioeconomic deprivation§
Quintile 1 (least deprived) 7373 (10·5%) 4268 (10·9%) 3105 (9·9%)
Quintile 2 9765 (13·9%) 5528 (14·2%) 4237 (13·5%)
Quintile 3 12 560 (17·9%) 6820 (17·5%) 5740 (18·4%)
Quintile 4 16 522 (23·5%) 8492 (21·7%) 8030 (25·7%)
Quintile 5 (most deprived) 24 100 (34·3%) 13 937 (35·7%) 10 163 (32·5%)
Pregnancy risk factors¶
Pre-existing diabetes 1021 (1·5%) 502 (1·3%) 519 (1·7%)
Pre-existing hypertensive
conditions
488 (0·7%) 250 (0·6%) 238 (0·8%)
Gestational diabetes|| 4294 (6·4%) 2263 (6·1%) 2031 (6·8%)
Pre-eclampsia or eclampsia 1442 (2·1%) 779 (2·0%) 663 (2·1%)
Highest level of pre-pregnancy secondary mental health-care contact
Community care 53 098 (75·5%) 28 880 (74·0%) 24 218 (77·4%)
Crisis resolution team 13 832 (19·7%) 8242 (21·1%) 5590 (17·9%)
Hospital admission 3393 (4·8%) 1925 (4·9%) 1468 (4·7%)
Timing of most recent pre-pregnancy secondary mental health-care contact, years
>5 18 302 (26·0%) 10 219 (26·2%) 8083 (25·8%)
1–5 34 672 (49·3%) 19 770 (50·6%) 14 902 (47·7%)||
<1 17 349 (24·7%) 9058 (23·2%) 8291 (26·5%)
Data are n (%). *Missing n=6 (<1%). †Missing n=3589 (5·1%). ‡Missing n=7843 (11·2%). §Missing n=3 (<1%). ¶Missing
n=3589 (5·1%). ||For each characteristic, the percentages were calculated only in women with non-missing data, which
explains apparent discrepancies in percentages for gestational diabetes.
Table 1: Baseline characteristics of women according to the regional availability of a community
perinatal mental health team
 6
6
 7
7
 8
8
 9
9
1
/
9
100%