Control, coordination and homeostasis
Homeostasis literally means “same state” and it refers to the process of keeping the internal body
environment in a steady state
the hormone system and the nervous system is dedicated to homeostasis
• All homeostatic mechanisms use negative feedback to maintain a constant value (called the set point)
• Negative feedback means that whenever a change occurs in a system, the change automatically
causes a corrective mechanism to start, which reverses the original change and brings the system
back to normal
Excretion and homeostasis
• Excretion means the removal of metabolic waste products from cells.
• Carbon dioxide and urea are the common wastes
• Lung excrete carbon dioxide
• Kidney excrete urea
• Urea is produced in liver through deamination (removing nitrogen atom from excessive amino acids)
Amino acid metabolism takes place in the liver
1. Deamination
• In this reaction an amino group is removed from an amino acid to form ammonia and a keto acid.
2. Urea Synthesis
In this reaction ammonia is converted to urea, ready for excretion by the kidney
• The kidney remove urea and other toxic wastes from the blood, forming a dilute solution called urine
in the process.
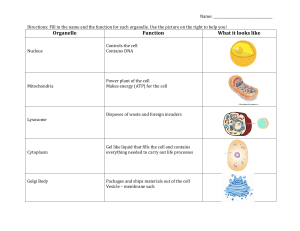
Kidney makes urine in two stage :
• Ultrafiltration (involves filtering small molecules out of blood into the renal capsule)
• Reabsorption (involves taking back any useful molecules from the fluid in the nephron as it flows
along)

1. Renal capsule – Ultrafiltration
• The renal artery splits into numerous arterioles, each feeding a nephron.
• The arteriole splits into numerous capillaries, which form a knot called a glomerulus.
• The glomerulus is enclosed by the renal capsule (Bowman’s capsule)
• The arteriole leading into the glomerulus (the afferent arteriole) is wider than the one leading out (the
efferent arteriole)
• so there is high blood pressure in the capillaries of the glomerulus
• This pressure forces plasma out of the blood by ultrafiltration.
• Both the capillary walls and the capsule walls are formed from a single layer of flattened endothelial
cells with gaps between them
• Endothelial cells of renal capsule forms podocytes (cell with tiny projections, with gaps) at the sides
facing the glomerulus; other regions consists of squamous epithelial cells
• Basement membrane (network of collagen & glycoproteins) act as a filter
• all molecules with a molecular mass of <70000 are squeezed out of the blood to form a filtrate in the
renal capsule
• Only blood cells and large proteins remain in the blood
• The glomerular filtrate is identical to blood plasma but do not contain large plasma proteins

Factors affecting glomerular filtration rate
The rate at which fluid seeps from the blood in the glomerular capillaries into the renal capsule
• Differences in water potential
• Blood pressure is relatively high in glomerulus (difference in width of afferent arteriole and efferent
arteriole) raise water potential of blood plasma
• But concentration of solutes is higher in blood plasma as well
• Overall, the effect of differences in pressure outweighs the effect of the differences in solute
concentration
• Overall, the water potential of blood plasma in glomerulus is higher than the water potential of the
fluid in renal capsule
• Water continue to move down water potential gradient
2. Proximal Convoluted Tubule – selective reabsorption
• The proximal convoluted tubule is the longest (14mm) and widest (60µm) part of the nephron. It is
lined with epithelial cells containing microvilli and numerous mitochondria
• In this part of the nephron over 80% of the filtrate is reabsorbed into the tissue fluid and then to the
blood.
• This ensures that all the “useful” materials that were filtered out of the blood (such as glucose and
amino acids) are now returned to the blood.
• All glucose, all amino acids and 85% of mineral ions are reabsorbed by active transport from the
filtrate to the tissue fluid. They then diffuse into the blood capillaries.
• Small proteins are reabsorbed by pinocytosis, digested, and the amino acids diffuse into the blood.

• 80% of the water is reabsorbed to the blood by osmosis.
• Surprisingly, some urea is reabsorbed to the blood by diffusion.
• Urea is a small, uncharged molecule, so it can pass through membranes by lipid diffusion and there
isn’t much the kidney can do about it.
• Since this is a passive process, urea diffuses down its concentration gradient until the concentrations
of urea in the filtrate and blood are equal. So in each pass through the kidneys half the urea is
removed from the blood and half remains in the blood.
Reabsorption in the proximal convoluted tubule
• Basal membrane of the cells lining the proximal tubule actively transport sodium ions out of the cell
• The sodium ions are carried away by the blood
• Concentration of sodium ions inside the cell decrease
• Created a concentration gradient to allow diffusion of ions from the fluid in the lumen into the cells
• But need transporter proteins
• Transporter proteins transport ions with glucose or amino acids simultaneously
• The concentration gradient of sodium provides enough energy to pull in glucose/ amino acid
molecules active transport of glucose and amino acids
• As substances move, water follows by osmosis
3. Loop of Henle – Formation of a Salt Bath
The function of the loop of Henle is to create high concentration of salts in the tissue fluid of medulla
(kidney) to reabsorb water
• Loop of Henle conserve water in the body rather than lost in urine
• The first part of the loop – descending limb
• The second part of the loop – ascending limb

• The loop of Henle create concentration gradient by actively pumping sodium and chloride ions out of
the filtrate into the tissue fluid in the ascending limb (2nd part of the loop)
• The walls of the upper parts of the ascending limb is impermeable to water; this it the part where
active pumping of salts happen
• This raises the concentration of sodium and chloride ions in the tissue fluid of medulla
• causes water to leave descending limb
• The first part of the loop (the descending limb) is permeable to ions and water, but water leaves by
osmosis. This makes the filtrate more concentrated as it descends.
• The longer the loop, the more concentrated towards the bottom of the loop
• as the concentrated fluid now turns to flow up the ascending limb, sodium and chloride ions leave
readily down concentration gradient
• As the fluid continues up the ascending limb, it becomes gradually less concentrated
• Having the two limbs running side by side, the fluid flowing down in one and up in one enables
the maximum concentration to be built up both inside and outside the tube at the bottom of the loop
• This mechanism is known as a counter-current multiplier
4. Distal Convoluted tubule – Homeostasis and Secretion
• It is relatively short and has a brush border (i.e. microvilli) with numerous membrane pumps for
active transport.
• In the distal convoluted tubule sodium ions are actively transported from the filtrate into tissue fluid
• Potassium ions are transported into the tubule
• Secretion of substances occurs here and it is regulated by hormones, so this is the homeostatic part of
the kidney.
• Substances secreted include H+ (for pH homeostasis), K+ (for salt homeostasis), ethanol, toxins,
drugs and other “foreign” substances.
 6
6
 7
7
 8
8
 9
9
 10
10
 11
11
 12
12
 13
13
 14
14
 15
15
 16
16
 17
17
 18
18
 19
19
 20
20
1
/
20
100%