UNIVERSITY OF CALGARY

UNIVERSITY OF CALGARY
Evaluating the Association between Estradiol and Quality of Life and Cardiovascular Risk and
Mortality in Healthy Women and Women with Chronic Kidney Disease
by
Sharanya Ramesh
A THESIS
SUBMITTED TO THE FACULTY OF GRADUATE STUDIES
IN PARTIAL FULFILMENT OF THE REQUIREMENTS FOR THE
DEGREE OF DOCTOR OF PHILOSOPHY
GRADUATE PROGRAM IN MEDICAL SCIENCE
CALGARY, ALBERTA
AUGUST, 2016
© Sharanya Ramesh 2016

ii
Abstract
Chronic kidney disease (CKD) is associated with a poor quality of life and high risk of
cardiovascular (CV) mortality, specifically sudden cardiac death (SCD), and an upregulated
renin angiotensin system. Women with end stage kidney disease (ESKD) experience premature
menopause, and in healthy women menopause is correlated with a poor quality of life and higher
CV mortality. A series of studies was conducted in healthy women and women with CKD to
determine the associations between menopause status, serum estradiol and 1) cardiac autonomic
tone (CAT), a surrogate marker for SCD, in a high Angiotensin II (AngII) state 2) mortality in
women with ESKD and 3) quality of life(QoL) in women with CKD. We also summarized the
impressions of healthcare workers and patients on the discussion of symptoms of low sex
hormones in a clinical setting. In healthy men and women, sex hormones did not correlate with
baseline CAT; however, men with lower testosterone levels were unable to maintain CAT in
response to AngII. At baseline, postmenopausal women had a lower CAT in comparison to
premenopausal women. In response to AngII postmenopausal women and premenopausal
women in the luteal phase were unable to maintain their CAT. Through a survey of nephrologists
we found that nephrologists recognize the impact of CKD on sex hormones in women but report
infrequently discussing sex hormone related issues with patients. In a systematic review of
studies examining the effect of postmenopausal hormone therapy on CV outcomes in women
with ESKD, hormone therapy was associated with a favourable lipid profile. However, we found
that peri- and premenopausal women with ESKD on hemodialysis had a higher risk of all-cause,
cardiovascular and non-cardiovascular mortality compared to postmenopausal women.
Furthermore menopause specific QoL scores did not correlate with kidney function in CKD

iii
women. We found that associations between menopause status and CV risk and QoL in the CKD
population are complex. This body of work can be used for hypothesis generation for future
studies and trials aimed to determine the mediators of cardiovascular risk and poor quality of life
in this population.

iv
Acknowledgements
I am very thankful for the opportunity to have spent the past four years of my life
studying this important area of research, which I am very passionate about. This would not have
been possible without the support and guidance of incredible people. First, I would like to thank
my supervisor and my valued mentor, Dr. Sofia Ahmed, from the bottom of my heart. Her
unwavering support, mentorship, kindness, guidance, and trust have carried me through these
four years, and this thesis would not have been possible without her. I would also like to extend a
heartfelt thank you to my thesis committee members, Dr. Jayna Holroyd-Leduc, Dr. Stephen
Wilton, and Dr. Matthew James, for their commitment to my academic and personal
development, valuable input and time, and mentorship throughout the years.
To my parents, Mallika and Ramesh, thank you so much for instilling in me the values of
hard-work, resilience and a passion for learning, without your love and support I would not be
who I am today. A very special thank you to my sister, Sanjana, who has been my rock for the
past few years and who held my hand through many doubtful moments, you continue to amaze
me with your understanding and kindness. To my friends near and far, who have always been
there to keep me grounded and supported, I am so thankful for your uplifting messages, votes of
confidence and wonderful company.
Last but not least, I would like to express my deep gratitude to the patients who
volunteered to participate in my studies, and the nurses, nephrologists and administrators of the
Southern Alberta Renal Program who took the time out of their busy schedules to help with my
project. Your kindness will not be forgotten.

v
Table of Contents
Abstract ............................................................................................................................... ii
Acknowledgements ............................................................................................................ iv
Table of Contents .................................................................................................................v
List of Tables .................................................................................................................... vii
List of Figures and Illustrations ....................................................................................... viii
List of Symbols, Abbreviations and Nomenclature .............................................................x
CHAPTER ONE: INTRODUCTION ..................................................................................1
1.1 Chronic Kidney Disease ............................................................................................1
1.1.1 Chronic kidney disease prevalence and burden of disease ................................1
1.1.2 Physical and psychological symptoms of uremia ..............................................1
1.1.3 Reproductive dysfunction, sexual dysfunction and premature menopause in
women with CKD ..............................................................................................2
1.1.4 Cardiovascular (CV) mortality in chronic kidney disease ................................2
1.2 Menopause and the role of estradiol ..........................................................................4
1.2.1 Menopause associated poor quality of life and high cardiovascular risk ..........4
1.2.1.1 Menopause and quality of life .................................................................5
1.2.1.2 Menopause and cardiovascular risk .........................................................5
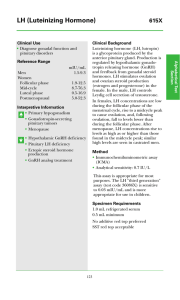
1.2.2 Estradiol .............................................................................................................6
1.2.3 Normal hypothalamus pituitary gonadal axis ....................................................6
1.2.4 Endogenous estradiol on quality of life .............................................................8
1.2.5 Cardioprotective role of endogenous estradiol ..................................................9
1.2.6 Cardiovascular risk and exogenous estradiol ..................................................10
1.2.7 WISE classification for menopausal status .....................................................12
1.3 Abnormalities in the hypothalamic pituitary gonadal axis in CKD .........................13
1.4 Assessment of Cardiovascular Risk, Quality of Life and Menopausal Symptoms .15
1.4.1 Heart rate variability (HRV) as a predictor of CVD risk ................................15
1.4.2 Using the Menopausal Specific Quality of Life (MENQOL) survey to determine
menopausal symptoms .....................................................................................17
1.5 Current state of the science ......................................................................................17
1.6 Objective ..................................................................................................................18
1.7 Thesis Outline ..........................................................................................................19
CHAPTER TWO: TESTOSTERONE IS ASSOCIATED WITH THE CARDIOVASCULAR
AUTONOMIC RESPONSE TO A STRESSOR IN HEALTHY MEN ...................20
CHAPTER THREE: CARDIAC AUTONOMIC RESPONSE TO ANGIOTENSIN II IN
HEALTHY PREMENOPAUSAL AND POSTMENOPAUSAL WOMEN ............39
CHAPTER FOUR: SEX HORMONE STATUS IN WOMEN WITH CHRONIC KIDNEY
DISEASE: SURVEY OF NEPHROLOGISTS’ AND RENAL ALLIED HEALTH
CARE PROVIDERS’ PERCEPTIONS. ...................................................................59
 6
6
 7
7
 8
8
 9
9
 10
10
 11
11
 12
12
 13
13
 14
14
 15
15
 16
16
 17
17
 18
18
 19
19
 20
20
 21
21
 22
22
 23
23
 24
24
 25
25
 26
26
 27
27
 28
28
 29
29
 30
30
 31
31
 32
32
 33
33
 34
34
 35
35
 36
36
 37
37
 38
38
 39
39
 40
40
 41
41
 42
42
 43
43
 44
44
 45
45
 46
46
 47
47
 48
48
 49
49
 50
50
 51
51
 52
52
 53
53
 54
54
 55
55
 56
56
 57
57
 58
58
 59
59
 60
60
 61
61
 62
62
 63
63
 64
64
 65
65
 66
66
 67
67
 68
68
 69
69
 70
70
 71
71
 72
72
 73
73
 74
74
 75
75
 76
76
 77
77
 78
78
 79
79
 80
80
 81
81
 82
82
 83
83
 84
84
 85
85
 86
86
 87
87
 88
88
 89
89
 90
90
 91
91
 92
92
 93
93
 94
94
 95
95
 96
96
 97
97
 98
98
 99
99
 100
100
 101
101
 102
102
 103
103
 104
104
 105
105
 106
106
 107
107
 108
108
 109
109
 110
110
 111
111
 112
112
 113
113
 114
114
 115
115
 116
116
 117
117
 118
118
 119
119
 120
120
 121
121
 122
122
 123
123
 124
124
 125
125
 126
126
 127
127
 128
128
 129
129
 130
130
 131
131
 132
132
 133
133
 134
134
 135
135
 136
136
 137
137
 138
138
 139
139
 140
140
 141
141
 142
142
 143
143
 144
144
 145
145
 146
146
 147
147
 148
148
 149
149
 150
150
 151
151
 152
152
 153
153
 154
154
 155
155
 156
156
 157
157
 158
158
 159
159
 160
160
 161
161
 162
162
 163
163
 164
164
 165
165
 166
166
 167
167
 168
168
 169
169
 170
170
 171
171
 172
172
 173
173
 174
174
 175
175
 176
176
 177
177
 178
178
 179
179
 180
180
 181
181
 182
182
 183
183
 184
184
 185
185
 186
186
 187
187
 188
188
 189
189
 190
190
 191
191
 192
192
 193
193
 194
194
 195
195
 196
196
 197
197
 198
198
1
/
198
100%