206162Orig1s000 MEDICAL REVIEW(S) CENTER FOR DRUG EVALUATION AND RESEARCH

CENTER FOR DRUG EVALUATION AND
RESEARCH
APPLICATION NUMBER:
206162Orig1s000
MEDICAL REVIEW(S)

CLINICAL REVIEW
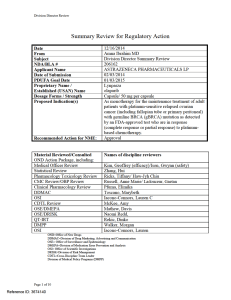
Application Type NDA
Application Number(s) 206162
Priority or Standard Priority
Submit Date(s) 2/3/14
Received Date(s) 2/3/14
PDUFA Goal Date 1/3/15
Division / Office DOP1/OHOP
Reviewer Name(s) Amy McKee CDTL
Geoffrey Kim (efficacy)
Gwynn Ison (safety)
Review Completion Date 12/2/14
Established Name Olaparib/AZD2281
(Proposed) Trade Name LynparzaTM
Therapeutic Class PARP inhibitor
Applicant AstraZeneca
Formulation(s) Oral
Dosing Regimen 400 mg BID
Indication(s) Monotherapy in patients with deleterious or
suspected deleterious germline BRCA mutated (as
detected by an FDA-approved test) advanced
ovarian cancer who have been treated with three or
more prior lines of chemotherapy.
Template Version: March 6, 2009
Reference ID: 3666348

Clinical Review
Geoffrey Kim and Gwynn Ison
NDA 206162
Lynparza (olaparib)
2
Table of Contents
1 RECOMMENDATIONS/RISK BENEFIT ASSESSMENT .............................................. 9
1.1 Recommendation on Regulatory Action .......................................................................... 9
1.2 Risk Benefit Assessment .................................................................................................. 9
1.3 Recommendations for Postmarket Risk Evaluation and Mitigation Strategies .............. 11
1.4 Recommendations for Postmarket Requirements and Commitments ............................ 12
CLINICAL POST MARKETING REQUIREMENTS: ......................................................... 12
2 INTRODUCTION AND REGULATORY BACKGROUND .......................................... 12
2.1 Product Information ........................................................................................................ 12
2.2 Tables of Currently Available Treatments for Proposed Indications ............................. 13
2.3 Availability of Proposed Active Ingredient in the United States ................................... 14
2.4 Important Safety Issues with Consideration to Related Drugs ....................................... 14
2.5 Summary of Presubmission Regulatory Activity Related to Submission ...................... 15
2.6 Other Relevant Background Information ....................................................................... 16
Ovarian Cancer ......................................................................................................................... 16
BRCA ........................................................................................................................................ 16
3 ETHICS AND GOOD CLINICAL PRACTICES ............................................................ 17
3.1 Submission Quality and Integrity ................................................................................... 18
3.2 Compliance with Good Clinical Practices ...................................................................... 18
3.3 Financial Disclosures ...................................................................................................... 18
4 SIGNIFICANT EFFICACY/SAFETY ISSUES RELATED TO OTHER REVIEW
DISCIPLINES ...................................................................................................................... 19
4.1 Chemistry Manufacturing and Controls ......................................................................... 19
4.2 Clinical Microbiology..................................................................................................... 19
4.3 Preclinical Pharmacology/Toxicology ........................................................................... 19
4.4 Clinical Pharmacology ................................................................................................... 19
4.4.1 Mechanism of Action .............................................................................................. 20
4.4.2 Pharmacodynamics .................................................................................................. 20
4.4.3 Pharmacokinetics ..................................................................................................... 20
5 SOURCES OF CLINICAL DATA ..................................................................................... 20
5.1 Tables of Studies/Clinical Trials .................................................................................... 20
5.2 Review Strategy .............................................................................................................. 21
5.3 Discussion of Individual Studies/Clinical Trials ............................................................ 21
5.3.1 Study Design.................................................................................................................. 22
5.3.2 Study Drug Administration and Schedule ...................................................................... 23
5.3.3 Study Endpoints .............................................................................................................. 23
5.3.4 Eligibility Criteria .......................................................................................................... 23
5.3.5 Duration of Treatment .................................................................................................... 24
5.3.6 Primary Endpoint Evaluation ........................................................................................ 24
Reference ID: 3666348

Clinical Review
Geoffrey Kim and Gwynn Ison
NDA 206162
Lynparza (olaparib)
3
5.3.8 Major Protocol Amendments......................................................................................... 26
6 REVIEW OF EFFICACY .................................................................................................. 26
Efficacy Summary .................................................................................................................... 26
6.1 Indication ........................................................................................................................ 26
6.1.1 Methods ................................................................................................................... 27
6.1.2 Demographics .......................................................................................................... 27
6.1.3 Subject Disposition .................................................................................................. 29
6.1.4 Analysis of Primary Endpoint(s) ............................................................................. 29
6.1.5 Analysis of Secondary Endpoints(s) ....................................................................... 30
6.1.6 Other Endpoints ....................................................................................................... 31
6.1.7 Subpopulations ........................................................................................................ 31
6.1.8 Analysis of Clinical Information Relevant to Dosing Recommendations .............. 31
6.1.9 Discussion of Persistence of Efficacy and/or Tolerance Effects ............................. 31
6.1.10 Additional Efficacy Issues/Analyses ....................................................................... 35
7 REVIEW OF SAFETY ....................................................................................................... 39
Safety Summary ........................................................................................................................ 39
7.1 Methods .......................................................................................................................... 39
7.1.1 Studies/Clinical Trials Used to Evaluate Safety ...................................................... 39
7.1.2 Categorization of Adverse Events ........................................................................... 40
7.1.3 Pooling of Data Across Studies/Clinical Trials to Estimate and Compare Incidence
................................................................................................................................. 41
7.2 Adequacy of Safety Assessments ................................................................................... 42
7.2.1 Overall Exposure at Appropriate Doses/Durations and Demographics of Target
Populations .............................................................................................................. 43
7.2.2 Explorations for Dose Response ............................................................................. 44
7.2.3 Special Animal and/or In Vitro Testing .................................................................. 44
7.2.4 Routine Clinical Testing .......................................................................................... 44
7.2.5 Metabolic, Clearance, and Interaction Workup ....................................................... 44
7.2.6 Evaluation for Potential Adverse Events for Similar Drugs in Drug Class ............ 44
7.3 Major Safety Results ...................................................................................................... 44
7.3.1 Deaths ...................................................................................................................... 44
7.3.2 Nonfatal Serious Adverse Events ............................................................................ 49
7.3.3 Dropouts and/or Discontinuations ........................................................................... 53
7.3.4 Significant Adverse Events ..................................................................................... 54
3. Pneumonitis ............................................................................................................. 65
7.3.5 Submission Specific Primary Safety Concerns ....................................................... 67
7.4 Supportive Safety Results ............................................................................................... 67
7.4.1 Common Adverse Events ........................................................................................ 67
7.4.2 Laboratory Findings ................................................................................................ 69
7.4.3 Vital Signs ............................................................................................................... 71
7.4.4 Electrocardiograms (ECGs) .................................................................................... 72
7.4.5 Special Safety Studies/Clinical Trials ..................................................................... 73
Reference ID: 3666348

Clinical Review
Geoffrey Kim and Gwynn Ison
NDA 206162
Lynparza (olaparib)
4
Renal impairment .................................................................................................................. 74
7.4.6 Immunogenicity ....................................................................................................... 76
7.5 Other Safety Explorations .............................................................................................. 76
7.5.1 Dose Dependency for Adverse Events .................................................................... 76
7.5.2 Time Dependency for Adverse Events .................................................................... 77
7.5.3 Drug-Demographic Interactions .............................................................................. 78
7.5.4 Drug-Disease Interactions ....................................................................................... 79
7.5.5 Drug-Drug Interactions ........................................................................................... 79
7.6 Additional Safety Evaluations ........................................................................................ 79
7.6.1 Human Carcinogenicity ........................................................................................... 79
7.6.2 Human Reproduction and Pregnancy Data ............................................................. 80
7.6.3 Pediatrics and Assessment of Effects on Growth .................................................... 80
7.6.4 Overdose, Drug Abuse Potential, Withdrawal and Rebound .................................. 80
7.7 Additional Submissions / Safety Issues .......................................................................... 80
8 POSTMARKET EXPERIENCE ........................................................................................ 80
9 APPENDICES ...................................................................................................................... 81
9.1 Literature Review/References ........................................................................................ 81
9.2 Labeling Recommendations ........................................................................................... 83
9.3 Advisory Committee Meeting ........................................................................................ 83
EXECUTIVE SUMMARY ........................................................................................................ 87
BACKGROUND ......................................................................................................................... 88
Ovarian Cancer ......................................................................................................................... 88
BRCA ........................................................................................................................................ 89
Approved Therapies .................................................................................................................. 89
Major Regulatory Milestones for Olaparib Development ........................................................ 90
DESIGN OF THE MAJOR EFFICACY TRIAL (STUDY 19) .............................................. 91
Key Inclusion Criteria ............................................................................................................... 91
Key Exclusion Criteria .............................................................................................................. 91
Randomization .......................................................................................................................... 91
Treatment .................................................................................................................................. 92
Assessments .............................................................................................................................. 92
Safety Evaluation ...................................................................................................................... 92
Study Efficacy Endpoints ......................................................................................................... 93
Statistical Methods .................................................................................................................... 93
Amendments to the Statistical Analysis Plan ........................................................................... 93
STUDY 19 GBRCAM PATIENT DEMOGRAPHICS ........................................................... 94
STUDY 19 EFFICACY ANALYSES ........................................................................................ 96
Efficacy Outcomes .................................................................................................................... 96
Key Secondary Endpoints ......................................................................................................... 99
Reference ID: 3666348
 6
6
 7
7
 8
8
 9
9
 10
10
 11
11
 12
12
 13
13
 14
14
 15
15
 16
16
 17
17
 18
18
 19
19
 20
20
 21
21
 22
22
 23
23
 24
24
 25
25
 26
26
 27
27
 28
28
 29
29
 30
30
 31
31
 32
32
 33
33
 34
34
 35
35
 36
36
 37
37
 38
38
 39
39
 40
40
 41
41
 42
42
 43
43
 44
44
 45
45
 46
46
 47
47
 48
48
 49
49
 50
50
 51
51
 52
52
 53
53
 54
54
 55
55
 56
56
 57
57
 58
58
 59
59
 60
60
 61
61
 62
62
 63
63
 64
64
 65
65
 66
66
 67
67
 68
68
 69
69
 70
70
 71
71
 72
72
 73
73
 74
74
 75
75
 76
76
 77
77
 78
78
 79
79
 80
80
 81
81
 82
82
 83
83
 84
84
 85
85
 86
86
 87
87
 88
88
 89
89
 90
90
 91
91
 92
92
 93
93
 94
94
 95
95
 96
96
 97
97
 98
98
 99
99
 100
100
 101
101
 102
102
 103
103
 104
104
 105
105
 106
106
 107
107
 108
108
 109
109
 110
110
 111
111
 112
112
 113
113
 114
114
 115
115
 116
116
 117
117
 118
118
 119
119
 120
120
 121
121
 122
122
 123
123
 124
124
 125
125
 126
126
 127
127
 128
128
 129
129
 130
130
 131
131
1
/
131
100%



![Poster LIBER san antonio 2011 [Mode de compatibilité]](http://s1.studylibfr.com/store/data/000441925_1-0f624c1012097e18f69fca01a2951eb6-300x300.png)



