Cancero_dig_2010_2_4 supp


S2 3rd Congress of the African Middle Eastern Digestive Cancer Alliance
Table of contents
Celebrate with us the 10th course of the WGO Rabat training centre,
Meinhard Classen, GuidoTytgat............................................ S3
Celebration of the 10th anniversary of the Gastroenterology
and HepatologyTraining Course,Richard Kozarek ............................ S5
Partnership of the WGO Rabat training Centre .............................. S6
Come to Rabat on February 4 and 5, Meinhard Classen ....................... S7
Welcome to the 10th anniversary of the WGO-RTC,Naïma Amrani ............ S8
Acknowledgements...................................................... S10
3d Congress of the African Middle Eastern Digestive Cancer:
scientific and technical organisation......................................... S11
Scientific programme .................................................... S12
Abstracts .............................................................. S15
Posters................................................................ S46
Poster session information ................................................ S98
Congress information .................................................... S99
Cancéro digest – Editorial Board........................................... S101
Cancéro digest – Instructions to authors.................................... S102
Conference hall ........................................................ S103
City map of Rabat ....................................................... S104

3rd Congress of the African Middle Eastern Digestive Cancer Alliance S3
Celebrate with us the 10th course
of the WGO-Rabat training center!
Almost 10 yearsago,through the initiativeand
dedicated butcareful negotiations of Prof
Meinhard Classen from Munich the Rabat WGO
training center was created under the energetic
leadership of its director Prof. Naïma Amrani.We
all were present at the inauguration and could not
foresee at that time that Rabat would become the
pearl of theWGO-training centers.The facilities of
the center are superb and ideally suited for small
and larger group discussion and hand-on training
sessions.
This is now already the tenth Rabat training center
course and looking back, we all have witnessed
the steady educational progress and the rising
enthusiasm of the participants largely from
francophone Africa, diligently selected by Prof.
Amrani.To be truly appreciated is the dedication
with which Prof. Amrani and her team design an
equilibrated educational program, adapted to
local unmet needs, yet incorporating all novel
developments in Hepato-gastroenterology,offering
a balanced mix of theoretical teaching and
practical hands-on training, also applauded by a
most distinguished foreign faculty over the years.
To measure the actual impact of the center
activities on medical care in the homelands remains
utterly difficult, butevenwithout having exact
figures, one can be assured that the impact is real
and substantial. Bringing novelinsights in hepato-
gastroenterology science and practice together
with renewed professional enthusiasm, even to
the most remote areas of (francophone) Africa is
bound to raise the level of medical care and will
contribute in narrowing the gap between emerging
and developed countries, aworld of solidarity!
What more can we do than to wish the Rabat
center,its director and coworkers a long, happy
and prosperous life, with continued building and
expansion and belief in its precious educational
role particularly in the discipline of Hepato-
gastroenterology,so dear to our hearts. May the
2010 course expand and refresh knowledge and
invigorate enthusiasm in all its participants, to be
long remembered.
On behalf of Prof M Classen and Prof GNJTytgat

S4 3rd Congress of the African Middle Eastern Digestive Cancer Alliance
Advisory Council 2010-2013
Executive committee
Co-chair (to 2010) Sidney Winawerwinawers@MSKCC.org
Co-chair GuidoTytgat g.n.tytgat@amc.nl
Officers Thomas Seufferlein thomas.seuffer[email protected]
Meinhard Classen [email protected]
Joseph Geenen [email protected]
Linda Rabeneck Linda.Rabeneck@sw.ca
Wolff Schmiegel wolff.schmiegel@ruhr-uni-bochum.de
Eric van Cutsem Eric.V[email protected].be
OfficerWGO President Richard Kozarek Richard.Kozarek@vmmc.org
Councillors Carolyn Aldige Carolyn.Aldige@preventcancer.org
Alberto Montorialberto.montori@alice.it
Bernard Levin bl[email protected]
Christa Maar [email protected]
Robert Smith robert.smith@cancer.org
GraemeYo ung graeme.young@flinders.edu.au
Wei-ChengYo uweichengyou@yahoo.com
San Ren Lin [email protected]
Naima Amrani n.amr[email protected]
Ann Zauber zauber[email protected]g
Maria Elena Martinez emartinez@azcc.arizona.edu
René LambertLambert@iarc.fr
Angelita Habr-Gama [email protected]
Vladimir Ivashkin gastro@orc.ru
Masaki Kitajima kitajima@sc.itc.keio.ac.jp
Ibrahim Mostafa ibrahimmostafa@egyptgastrohep.com
Antoni Castells CASTELLS@clinic.ub.es
Enrique Quintero [email protected]
Asadur J.Tchekmedyian [email protected]g.uy
Nadir Arber [email protected].il
Philippe Rougier rougier.philippe@wanadoo.fr
Joseph Sung [email protected]
KL. Goh [email protected]
E. Kuiperse.t.kuipers@senter.nl
Pedro Llorens Sabate [email protected]

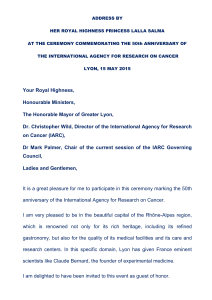
3rd Congress of the African Middle Eastern Digestive Cancer Alliance S5
Celebration of the 10th anniversary
of the Gastroenterology
and HepatologyTraining Course
WGO is very proud of the accomplishments of the Rabat Training
Centre,and in particular,the excellence of training that has been
and continues to be provided by the Centre to physicians living and
working in the northwestern region of Africa and nearby locales.
Representing the culmination of 10 years of success in training, the
annual Gastroenterology and Hepatology Tr aining Course is but
one aspect of the broad range of initiatives undertaken in Rabat
that have significantly impacted the knowledge and expertise of
physicians in a region where the need for education and training in
gastroenterology is profound.Yo u are to be congratulated on your
vision and commitment in this regard.
We highly value our collaboration with the Training Centre in Rabat
and look forward to continuing our successful partnership in the
years to come.
With warmest regards,
Richard Kozarek, MD
President
World Gastroenterology Organisation
 6
6
 7
7
 8
8
 9
9
 10
10
 11
11
 12
12
 13
13
 14
14
 15
15
 16
16
 17
17
 18
18
 19
19
 20
20
 21
21
 22
22
 23
23
 24
24
 25
25
 26
26
 27
27
 28
28
 29
29
 30
30
 31
31
 32
32
 33
33
 34
34
 35
35
 36
36
 37
37
 38
38
 39
39
 40
40
 41
41
 42
42
 43
43
 44
44
 45
45
 46
46
 47
47
 48
48
 49
49
 50
50
 51
51
 52
52
 53
53
 54
54
 55
55
 56
56
 57
57
 58
58
 59
59
 60
60
 61
61
 62
62
 63
63
 64
64
 65
65
 66
66
 67
67
 68
68
 69
69
 70
70
 71
71
 72
72
 73
73
 74
74
 75
75
 76
76
 77
77
 78
78
 79
79
 80
80
 81
81
 82
82
 83
83
 84
84
 85
85
 86
86
 87
87
 88
88
 89
89
 90
90
 91
91
 92
92
 93
93
 94
94
 95
95
 96
96
 97
97
 98
98
 99
99
 100
100
 101
101
 102
102
 103
103
 104
104
1
/
104
100%