O084 Oral Session Emerging resistance in fungi

O084
Oral Session
Emerging resistance in fungi
CIRCULATION OF MOULDS BETWEEN CLINICAL AND ENVIRONMENTAL RESERVOIRS IN A
COPD PATIENT POPULATION: EMERGENCE OF ASPERGILLUS FUMIGATUS AZOLE-
RESISTANCE IN THE NORTH OF FRANCE
C. Dauchy1, A. Standaert-Vitse2, O. Le Rouzic3, S. Nseir4, E. Dei-Cas2, E.M. Aliouat2, S. Fry3, E.
Frealle2
1Laboratoire de Parasitologie-Mycologie, CHRU de Lille & Faculté de Médecine de Lille Univ. Lille Nord
de France, Lille, France ; 2Biologie et Diversité des Pathogènes Eucaryotes Emergents (BDPEE),
Institut Pasteur de Lille Centre d'Infection et d'Immunité de Lille (CIIL) INSERM U1019 CNRS UMR 8204
Univ. Lille Nord de France, Lille, France ; 3Clinique des Maladies Respiratoires, CHRU de Lille & Faculté
de Médecine de Lille Univ. Lille Nord de France, Lille, France ; 4Pôle de Réanimation, CHRU de Lille &
Faculté de Médecine de Lille Univ. Lille Nord de France, Lille, France
Background: The emergence of azole resistance in Aspergillus fumigatus has been reported in azole-
exposed patients, but also in azole-naïve patients and in the environment, suggesting both long-term
azole therapy and the use of azole fungicides in agriculture could be involved in drug resistance
emergence. The main resistance mechanism implicates point mutations in the 14a-sterol demethylase
gene (cyp51A) and/or increased cyp51A expression due to a tandem repeat (TR) promoter alteration.
In this study, Aspergillus colonization prevalence and domestic mould exposure level were determined
in an azole-naïve COPD patient population. A. fumigatus clinical and environmental isolates were
characterized by cyp51A sequencing in order to clarify the circulation of A. fumigatus mutated isolates
between clinical and environmental reservoirs.
Methods: Sputa from 33 COPD patients that were admitted to the Pneumology Department of Lille
University Hospital (France) were prospectively collected from August 2011 to July 2013 for fungal
detection by culture and Aspergillus qPCR. For each patient, domestic mould exposure level was
determined by culture (colony counting) using an electrostatic dust fall collector (EDC) that had been
exposed for 10 weeks in the patient’s bedroom. Clinical and environmental samples were further
cultured on itraconazole-containing Sabouraud agar medium for azole-resistant isolates selection when
more than 10 A. fumigatus isolates were detected. Detection of cyp51A alterations was performed by
cyp51A sequencing for all A. fumigatus clinical and environmental isolates.
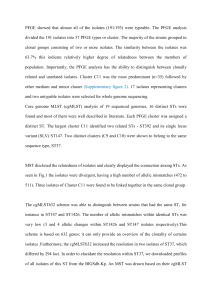
Results: The inclusion of 33 COPD patients yielded 31 sputa and 29 EDCs. Aspergillus colonization
was detected in 10 patients (32.2%) by culture and/or qPCR. Mould level in EDCs varied from 1 to 101
colonies. A. fumigatus was detected in 12 EDCs (41.4%) (1 to 19 colonies) from 1 A. fumigatus
colonized patient, 1 Aspergillus qPCR positive patient and 10 non-colonized patients. Cyp51A
sequencing in 25 A. fumigatus clinical and 34 environmental isolates revealed the presence of
F46Y/M172V/N248T/D255E/E427K mutated isolates in 3 clinical isolates from 2 patients. TR34/L98H
mutation was detected in 2 out of 34 environmental isolates (5.9%) from 2 different patients, yielding a
6.9% prevalence of TR34/L98H A. fumigatus isolates in patient’s homes and a 16.7% prevalence in A.
fumigatus culture positive EDCs. In both TR34/L98H A. fumigatus positive EDCs, another mutated
isolate was detected, one exhibiting the F46Y/M172V/N248T/D255E/E427K mutation and the other one
a H285Y mutation.
Conclusion: This is the first report of TR34/L98H A. fumigatus isolates in the North of France. The
detection of cyp51A mutated isolates in environmental samples supports the role of agricultural azoles
in the emergence azole-resistance.
1
/
1
100%