Hirschsprung's & Anorectal Malformation: A Systematic Review
Telechargé par
Duy Linh Nguyễn

Vol.:(0123456789)
1 3
Pediatric Surgery International
https://doi.org/10.1007/s00383-019-04580-4
ORIGINAL ARTICLE
Concurrent Hirschsprung’s disease andanorectal malformation:
asystematic review
HirokiNakamura1· PremPuri1,2
Accepted: 12 September 2019
© Springer-Verlag GmbH Germany, part of Springer Nature 2019
Abstract
Background/purpose Hirschsprung’s disease (HSCR) and anorectal malformation (ARM) are often associated with other
congenital malformations, but the association of each other is rare. Some studies havereported the incidence of HSCR
associated with ARM ranging from 2.0 to 3.4%. The purpose of this study was to update the current epidemiological and
therapeutic features of this rare congenital association.
Methods A systematic literature search for relevant articles was performed in four databases using acombination of thefol-
lowing terms “association of Hirschsprung’s disease and anorectal malformation”, “aganglionosis and anorectal malforma-
tion” and “congenital megacolon and anorectal malformation” for studies published between 1952 and 2019. Reference lists
were screened for additional cases.
Results Forty-three studies met the defined inclusion criteria, reporting a total of 126 patients who were diagnosed with
HSCR with ARM. Thirty articles reported 42 single case reports of this association. Twelve articles reported 66 cases of
HSCR in case series of 3309 ARM patients, resulting in an incidence of 2% of this association. Associated syndrome was
foundin 25 cases (20%): Currarino syndrome in 11, Down syndrome in 8, Cat eye syndrome in 4 and Pallister–Hall syndrome
in 2 patients. Extent of aganglionosis was reported in 62 cases: short or rectosigmoid aganglionosis was reportedin 44, long
segment aganglionosis in 8, total colonic aganglionosis in 9 and total intestinal aganglionosis in 1 case.
Conclusion Although the association of ARM and HSCR is rare, the incidence of HSCR among ARM cases seems to be
higher than inthe general pediatric population. There wasa high incidence of coexistence of ARM and HSCR with severe
associated syndromes.
Keywords Hirschsprung’s disease· Anorectal malformation· Associated syndromes
Introduction
Hirschsprung’s disease (HSCR) and anorectal malformation
(ARM) are often associated with other congenital malforma-
tions encountered in pediatric surgery, with an incidence of
1:5000 live births, but the association of both disease is rare
[1–5]. The incidence of HSCR associated with ARM have
been reported ranging from 2.0 to 3.4% [6, 7]. The purpose
of this study was to update the current epidemiological and
therapeutic features of this rare congenital association.
Materials andmethods
A systematic review and meta-analysis were conducted
based on Preferred Reporting Items for Systematic Reviews
and Meta-Analyses (PRISMA) guidelines. A systematic
search of the literature was performed in the Pubmed,
Embase, Medline and Cochrane Library electronic data-
base for the keywords “association of Hirschsprung’s disease
and anorectal malformation”, “aganglionosis and anorec-
tal malformation” and “congenital megacolon and anorec-
tal malformation” for studies published between 1952 and
2019. There was no restriction regarding the language of
the publications. Reference lists of relevant articles were
* Prem Puri
1 National Children’s Research Centre, Our Lady’s Children’s
Hospital, Dublin, Ireland
2 School ofMedicine andMedical Science andConway
Institute ofBiomolecular andBiomedical Research
University College Dublin, Dublin, Ireland

Pediatric Surgery International
1 3
manually searched for further cohorts. Duplicates were
deleted. Resulting publications were reviewed in detail for
epidemiology, operative treatment, morbidity and clinical
outcome. The relevant articles were reviewed by title, key-
words and abstract by the authors (H. N. and P. P.) and a
full-text assessment of selected articles was performed.
Results
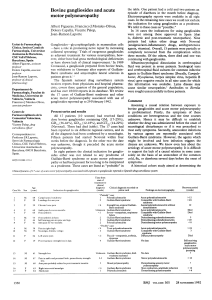
The initial search yielded a total of 239 publications, of
which 236 were identified by electronic database searching
and 3 from cross-referencing (Fig.1). After removal of 85
duplicate listed articles, 154 titles, keywords and abstracts
were screened. Of these, 102 non-relevant studies were
excluded. The remaining 52 publications were assessed in
full-text for eligibility and 9 articles were excluded because
they did not address any of the selection criteria. In total,
data from 43 studies (published between 1952 and 2019) met
defined inclusion criteria and was included in the cumulative
analysis [1, 6–48].
Forty-three studies met the defined inclusion crite-
ria, reporting a total of 126 patients who were diagnosed
with HSCR with ARM. Thirty articles reported 42 single
case reports of this association. Twelve articles reported
66 cases of HSCR in case series of 3309 ARM patients,
resulting in an incidence of 2% of this association. Associ-
ated syndrome was reportedin 25 cases (20%): Currarino
syndrome in 11, Down syndrome in 8, Cat eye syndrome
in 4 and Pallister–Hall syndrome in 2 patients (Table1).
Extent of aganglionosis was reported in 62 cases: short
or rectosigmoid aganglionosis in 44, long segment agan-
glionosis in 8, total colonic aganglionosis in 9 and total
intestinal aganglionosis in 1 case (Table2).
The mean duration of the diagnosis of HSCR after ini-
tial diagnosis of ARM was 8months. The surgical treat-
ment of HSCR was reported in 45 patients. Different type
of pull-through procedures after correction of ARM (36
cases), sphincter myectomies (2 cases) and 7 patients
underwent only one pull-through operation for concurrent
HSCR and ARM correction.
Fig. 1 This is an information
flow diagram, demonstrating the
process of selection and exclu-
sion of articles from the litera-
ture search for the purposes of
systematic review

Pediatric Surgery International
1 3
Discussion
Both HSCR and ARM are relatively common congenital
anomalies encountered in pediatric surgery [1]. The asso-
ciation of both anomalies is very rare with an incidence
of2.0–3.4% [1]. This systematic review showed the inci-
dence of HSCR associated with ARM cases was 2.0%.
This result consisted of 1.26% HSCR cases in 398 patients
with ARM in India [46] to 3.4% HSCR cases in 296 cases
of ARM in an early survey of pediatric surgeons in the US
and Canada [6].
Of the 42 single cases, 23 cases (54.7%) have been
reported with the associated syndromes. This high inci-
dence of associated syndromes (e.g. Down syndrome,
Cat eye syndrome, Currarino triad and Pallister–Hall
syndrome) may be partly explained by the local genetic
pool of the patients studied [24, 45]. Teerlink etal. [45]
reported 18 ARM cases were diagnosed with HSCR,
whose outcomes may indicate some genetic component
resulting in both ARM and HSCR. In this review, two
cases had Pallister–Hall syndrome. Prenatal genetic test-
ing for Pallister–Hall syndrome identified a GLI3 het-
erozygous, apparently de novo novel nonsense mutation
[47]. Gastrointestinal malformations may occur in Pallis-
ter–Hall syndrome because GLI3 affects the SHH pathway,
which plays a role in development and signaling pathways
between layers of embryonic tissue [47, 49]. Animal mod-
els have suggested defects in SHH signaling pathway can
lead to genitourinary anomalies such as imperforate anus
[50] and dilation of the gastrointestinal tract similar to
HSCR [47, 49].
It is not easy to diagnose HSCR with ARM because
the underlying ARM may be masking classical HSCR
symptoms such as the delayed passage of meconium and
abdominal distension. Watanatittan etal. [41] reported
alarge series and concluded that the diagnosis was delayed
after full correction of ARM owing to atypical symptoma-
tology and radiological findings. Eltayeb etal. [7] reported
that five cases in their series had delayed diagnosis. The
patients had developed abdominal distention and progres-
sive constipation that were masked by the functioning
stoma done as a first stage of ARM corrections [7].
Hoffman etal. [1] reported that 88% of the HSCR patients
with ARM had continence after ARM and HSCR correc-
tion at the end of the followed-up period. Eltayeb etal. [7]
reported that 72% of patients showed continence scores were
fair or good. However, the limitation of this study is thatthe
mean follow-up period wasvery short, only36months.
Conclusion
Although the association of ARM and HSCR is rare, the
incidence of HSCR among ARM cases seems to be higher
than in thegeneral pediatric population. There was high inci-
dence of coexistence of ARM and HSCR with sever associ-
ated syndrome. It is important to have attention for rectal
biopsy for the patient with severe and progressive constipa-
tion after full correction of ARM.
Compliance with ethical standards
Conflict of interest The authors declare that they have no conflict of
interest.
References
1. Hofmann AD, Puri P (2013) Association of Hirschsprung’s dis-
ease and anorectal malformation: a systematic review. Pediatr
Surg Int 29:913–917
2. Levitt MA, Pena A (2007) Anorectal malformations. Orphanet J
Rare Dis 2:33
3. Mittal A, Airon RK, Magu S, Rattan KN, Ratan SK (2004) Asso-
ciated anomalies with anorectal malformation (ARM). Indian J
Pediatr 71:509–514
4. Stoll C, Alembik Y, Dott B, Roth MP (2007) Associated malfor-
mations in patients with anorectal anomalies. Eur J Med Genet
50:281–290
5. Ratan SK, Rattan KN, Pandey RM, Mittal A, Magu S, Sodhi PK
(2004) Associated congenital anomalies in patients with anorec-
tal malformations—a need for developing a uniform practical
approach. J Pediatr Surg 39:1706–1711
6. Kiesewetter WB, Sukarochana K, Sieber WK (1965) The fre-
quency of aganglionosis associated with imperforate anus. Sur-
gery 58:877–880
7. Eltayeb AA, Refaiy A. (2014) Association of Hirschsprung’s dis-
ease with anorectal malformations: the early alarming signs for
diagnosis and comorbidity related to this association. J Pediatr
Surg. https ://doi.org/10.1016/j.jpeds urg.2014.04.007
8. Harmston GJ (1951) Hirschsprung’s disease associated with anal
stenosis and subhepatic cecum. Rocky Mt Med J 48:29–33
Table 1 Associated syndrome in patients with HSCR and coexisting
ARM
Syndrome Number
Currarino syndrome 11
Down syndrome 8
Cat-eye syndrome 4
Pallister–Hall syndrome 2
Table 2 Extent of aganglionosis Type Number
Short or rectosigmoid 44
Long 8
Total colon 9
Total intestine 1

Pediatric Surgery International
1 3
9. Bacon HE, Sherman LF (1952) Surgical management of congeni-
tal malformations of the anus and rectum; report of one hundred
eleven cases. AMA Arch Surg 64:331–344
10. Ragins H, Van Prohaska J (1957) Megarectum. Ann Surg
145:249–253
11. Jimenez-Urueta P, Alvarado-Garcia R, Gallego-Grijalva J (2005)
Agangliosis del colon en pacientes con malformacion anorrectal.
Analisis de 5 casos Cir Ciruj 73:283–285
12. Amornfa J, Taecholarn C, Khaoroptham S (2005) Currarino syn-
drome: report of two cases and review of the literature. J Med
Assoc Thai 88:1697–1702
13. Arbell D, Gross E, Orkin B, Koplewitz BZ, Udassin R (2006)
Imperforate anus, malrotation, and Hirschsprung’s disease: a rare
and important association. J Pediatr Surg 41:1335–1337
14. Baltogiannis N, Mavridis G, Soutis M, Keramidas D (2003) Cur-
rarino triad associated with Hirschsprung’s disease. J Pediatr Surg
38:1086–1089
15. Clarke SA, Van der Avoirt A (1999) Imperforate anus,
Hirschsprung’s disease, and trisomy 21: a rare combination. J
Pediatr Surg 34:1874
16. Flageole H, Fecteau A, Laberge JM, Guttman FM (1996)
Hirschsprung’s disease, imperforate anus, and Down’s syndrome:
a case report. J Pediatr Surg 31:759–760
17. Hasse W (1976) Associated malformation with anal and rectal
atresiae. Prog Pediatr Surg 9:99–103
18. Haynes JH, Bagwell CE (2003) Hirschprung’s disease and imper-
forate anus in Pallister–Hall syndrome: a new association. J Pedi-
atr Surg 38:1411–1412
19. Isik N, Elmaci I, Gokben B, Balak N, Tosyali N (2010) Currarino
triad: surgical management and follow-up results of four [correc-
tion of three] cases. Pediatr Neurosurg 46:110–119
20. Kilickesmez O, Gol IH, Uzun M, Oruk C (2006) Complete famil-
ial Currarino triad in association with Hirschsprung’s disease:
magnetic resonance imaging features and the spectrum of ano-
rectal malformations. Acta Radiol 47:422–426
21. Lukong CS, Mshelbwala PM, Anumah MA, Ameh EA, Nmadu PT
(2012) Anorectal malformation coexisting with Hirschsprung’s
disease: a report of two patients. Afr J Paediatr Surg 9:166–168
22. Luo CC, Ming YC, Chu SM, Chao HC (2010) Rare association
of malrotation, imperforate anus and Hirschsprung’s disease in an
infant. Pediatr Int 52:e9–10
23. Mahboubi S, Templeton JM Jr (1984) Association of
Hirschsprung’s disease and imperforate anus in a patient with
"cat-eye" syndrome. A report of one case and review of the lit-
erature. Pediatr Radiol 14:441–442
24. Martucciello G, Torre M, Belloni E, Lerone M, Pini Prato A,
Cama A etal (2004) Currarino syndrome: proposal of a diagnostic
and therapeutic protocol. J Pediatr Surg 39:1305–1311
25. Mengistu AD (2006) Hirschsprung’s disease and imperforate anus
in a new born: unusual assocation. Ethiop Med J 44:81–83
26. Ohno K, Nakamura T, Azuma T, Nakaoka T, Takama Y, Hayashi
H etal (2013) Familial Currarino syndrome associated with
Hirschsprung disease: two cases of a mother and daughter. J Pedi-
atr Surg 48:233–238
27. Oshio T (2008) Imperforate anus, malrotation, and Hirschsprung’s
disease with double zonal aganglionosis: an extremely rare com-
bination. J Pediatr Surg 43:222–226
28. Poenaru D, Uroz-Tristan J, Leclerc S, Murphy S, Bensoussan AL
(1995) Imperforate anus, malrotation and Hirschsprung’s disease:
a rare association. Eur J Pediatr Surg 5:187–189
29. Sakaniwa M (1981) The association of an ano-rectal malformation
and aganglionosis. Jpn J Pediatr Surg 13:895–900
30. Sieber WK (1979) Hirschsprung’s disease. In: Ravitch MM,
Welch KJ, Benson CD (eds) Pediatric surgery. Year Book Medi-
cal Publishers, Chicago, London, pp 1035–1054
31. Sinha CK, Grewal A, Ward HC (2007) Short-segment
Hirschsprung’s disease, cat eye syndrome, and anorectal malfor-
mation: a unique association. J Pediatr Surg 42:1454–1456
32. Stevenson JK, Herron PW (1967) Hirschsprung’s disease: a rare
cause of constipation in patients following surgical correction of
imperforate anus. Report of two cases Am Surg 33:555–558
33. Takada Y, Aoyama K, Goto T, Mori S (1985) The association of
imperforate anus and Hirschsprung’s disease in siblings. J Pediatr
Surg 20:271–273
34. Ward J, Sierra IA, D’Croz E (1989) Cat eye syndrome associated
with aganglionosis of the small and large intestine. J Med Genet
26:647–648
35. Zundel S, Obermayr F, Schaefer JF, Fuchs J (2010) Hirschsprung
disease associated with total colonic agenesis and imperforate
anus—case report and review of the literature. J Pediatr Surg
45:252–254
36. Riker WL (1957) Diagnosis and treatment of aganglionosis of the
myenteric plexus. AMA Arch Surg 75:362–376
37. Brayton D, Norris WJ (1958) Further experiences with the treat-
ment of imperforate anus. Surg Gynecol Obstet 107:719–726
38. Parkkulainen KV, Hjelt L, Sulamaa M (1960) Anal atresia com-
bined with aganlionic megacolon. Acta Chir Scand 118:252–256
39. Santulli TV, Schullinger JN, Kiesewetter WB, Bill AH Jr (1971)
Imperforate anus: a survey from the members of the Surgical
Secton of the American Academy of Pediatrics. J Pediatr Surg
6:484–487
40. Ikeda K, Goto S (1986) Additional anomalies in Hirschsprung’s
disease: an analysis based on the nationwide survey in Japan. Z
Kinderchir 41:279–281
41. Watanatittan S, Suwatanaviroj A, Limprutithum T, Rattanasuwan
T (1991) Association of Hirschsprung’s disease and anorectal
malformation. J Pediatr Surg 26:192–195
42. Suomalainen A, Wester T, Koivusalo A, Rintala RJ, Pakarinen
MP (2007) Congenital funnel anus in children: associated
anomalies, surgical management and outcome. Pediatr Surg Int
23:1167–1170
43. Raboei EH (2009) Patients with anorectal malformation and
Hirschsprung’s disease. Eur J Pediatr Surg 19:325–327
44. Tong MC (1981) Anorectal anomalies: a review of 49 cases. Ann
Acad Med Singap 10:479–484
45. Teerlink CC, Bernhisel R, Cannon-Albright LA, Rollins MD
(2018) A genealogical assessment of familial clustering of ano-
rectal malformations. J Hum Genet 63:1029–1034
46. Pant N, Khan TR, Malhotra S, Kumar P, Dheer Y, Wakhlu A
(2018) Diagnostic suggestion and surgical consideration for
Hirschsprung’s disease associated with high anorectal malforma-
tion. Ann Pediatr Surg 14:78–82
47. Li MH, Eberhard M, Mudd P, Javia L, Zimmerman R, Khalek N
etal (2015) Total colonic aganglionosis and imperforate anus in a
severely affected infant with Pallister–Hall syndrome. Am J Med
Genet A 167A:617–620
48. Saleem MM, Alzuobi MN, Shahait AD (2014) Cat eye syndrome,
anorectal malformation, and Hirschsprung’s disease. J Indian
Assoc Pediatr Surg 19:119–120
49. Yang JT, Liu CZ, Villavicencio EH, Yoon JW, Walterhouse D,
Iannaccone PM (1997) Expression of human GLI in mice results
in failure to thrive, early death, and patchy Hirschsprung-like gas-
trointestinal dilatation. Mol Med 3:826–835
50. Mo R, Kim JH, Zhang J, Chiang C, Hui CC, Kim PC (2001)
Anorectal malformations caused by defects in sonic hedgehog
signaling. Am J Pathol 159:765–774
Publisher’s Note Springer Nature remains neutral with regard to
jurisdictional claims in published maps and institutional affiliations.
1
/
4
100%