ANATOMIC BASES OF MEDICAL, RADIOLOGICAL AND SURGICAL TECHNIQUES
Adnan Ozturk ÆCigdem Kutlu ÆNurcan Taskara
Aysin Cetiner Kale ÆBulent Bayraktar ÆAycicek Cecen
Anatomic and morphometric study of the arcade of Frohse in cadavers
Received: 4 July 2004 / Accepted: 20 January 2005 / Published online: 9 July 2005
Springer-Verlag 2005
Abstract The most superior part of the superficial layer
of the supinator muscle is named as the arcade of Frohse
(AF). The deep branch of the radial nerve runs under
this arch. The AF is reported to be the most common
structure causing entrapment neuropathy of the deep
branch of the radial nerve. The aim of our study was to
reveal the anatomical properties and especially mor-
phometric measurements of the AF in cadavers. This
study was performed on 55 cadaver upper extremities.
The AF was classified macroscopically as either tendi-
nous or membranous. The width, length and thickness
of the AF were measured as the dimensions of the AF.
The ‘‘distance AF’’ between the lateral epicondyle of the
humerus and the AF was measured. The ‘‘forearm
length’’ between the lateral epicondyle of the humerus
and the styloid process of the radius was measured. The
distance AF was divided by the forearm length to find
the ‘‘ratio AF’’. In 87% of the extremities the AF was
tendinous, and in 13% it was membranous. The mean
width, length and thickness of the AF were 10.13, 8.60
and 0.77 mm, respectively. The mean distance AF and
forearm length were 46.23 and 233.17 mm, respectively.
The mean ratio AF was 0.199 (approximately 1/5).
These measurements of the dimensions of the AF may
contribute to the anatomy of the AF. The surgeon may
find the predicted distance AF of any upper extremity by
dividing its forearm length by 5.
Keywords Arcade of Frohse ÆSupinator muscle Æ
Radial nerve ÆAnatomy ÆMorphometry
Introduction
The deep branch of the radial nerve (DBRN) runs be-
tween the superficial and deep parts of the supinator
muscle to enter the posterior compartment of the fore-
arm. Then, it continues as the posterior interosseous
nerve [12,27].
The most superior part of the superficial layer of the
supinator muscle may form a fibrous arch [22]. This arch
(arcade of Frohse, AF) was first described by Frohse
and Fra
¨nkel [6] in 1908. The DBRN runs under the AF,
and enters the plane between the two parts of the supi-
nator muscle [22].
Kopell and Thompson [9] initially reported the
entrapment of the DBRN by the AF in 1963. Capener
[2] recorded the vulnerability of the DBRN at the AF in
1966. Spinner [22] stated the compression of the DBRN
at the AF in 1968. The AF is reported to be the most
common structure causing entrapment neuropathy of
the DBRN [1,3,4,5,7,8,10,11,13,14,15,16,17,18,
19,20,21,23,24,25,26].
The aim of our study was to reveal the anatomical
properties and especially the morphometric measure-
ments of the AF in cadavers.
Materials and methods
This study was performed on 55 upper extremities of the
formalin-fixed human cadavers used for the routine
A. Ozturk (&)ÆB. Bayraktar
Department of Anatomy, Istanbul Medical Faculty,
Istanbul University, Capa, 34390 Istanbul, Turkey
E-mail: [email protected]
Tel.: +90-212-4142176
Fax: +90-212-6358522
C. Kutlu
Department of Internal Medicine,
Haseki Education and Research Hospital, Aksaray,
34200 Istanbul, Turkey
N. Taskara
Tuccarbasi Istasyon Caddesi, No 54/20, Erenkoy,
34738 Istanbul, Turkey
A. C. Kale
Department of Anatomy, Medical Faculty,
Ondokuz Mayis University, 55139 Samsun, Turkey
A. Cecen
Neurosurgical Clinic of Kartal Research and Teaching Hospital,
Kartal, 34865 Istanbul, Turkey
Surg Radiol Anat (2005) 27: 171–175
DOI 10.1007/s00276-005-0321-z

dissection courses in the Anatomy Department of the
Istanbul Medical Faculty, Istanbul University, Turkey
during 2000 and 2003. All the cadavers were Caucasian
men, and the causes of their death were the diseases of
the respiratory and cardiovascular systems. The mean
age of the cadavers was 51.54 years (range
32—76 years). There were no pathological findings in
the dissection region of the upper extremities. From the
available records it was not possible to obtain any
information about the dominant hand, occupation,
habits and sporting activities of the specimens.
All the upper extremities were carefully dissected. The
radial nerve and its two terminal branches, the supinator
muscle and the AF were identified in the anatomical
position. The tip of the lateral epicondyle of the humerus
and the tip of the styloid process of the radius were
marked. In this study, acupuncture needles (size 0.25 ·
25 mm) were used to mark the measuring points for
each measurement. All the measurements were made
manually and macroscopically on the upper extremities
in the anatomical position by two experienced anato-
mists (A.O., B.B.), with digital calipers (measuring range
300 mm, resolution 0.01 mm, maximum error 0.02 mm).
The anatomical structures of the supinator muscle,
radial nerve and its two terminal branches were observed
and recorded.
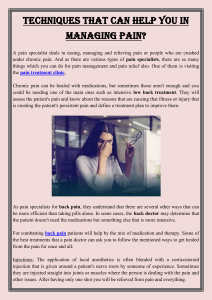
The anatomical structure of the AF was examined
macroscopically. First, the shape of the AF was re-
corded (Fig. 1a, b). Then, according to the classification
of Prasartritha et al. [15], the AF was classified: as ten-
dinous if the medial and lateral halves of the AF were
fibrous in texture (Fig. 1a), or as membranous if the
medial half of the AF was muscular (Fig. 1b). These two
types of the AF were photographed.
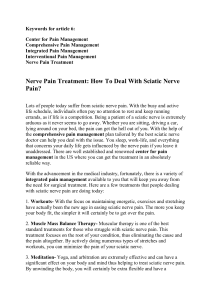
The width, length and thickness of the AF were
measured as the dimensions of the AF. The superolat-
eral tip of the AF was named as the proximal tip. The
inferomedial tip of the AF was named as the distal tip.
The proximal and distal tips were marked. First, four
imaginary lines were drawn to measure the width, length
and thickness of the AF (Fig. 2): (1) the first passed
horizontally from the proximal tip (the imaginary hori-
zontal line), (2) the second passed vertically from the
distal tip (the imaginary vertical line), (3) the third ex-
tended from the proximal tip to the distal tip (the
imaginary line connecting the two tips of the AF), and
(4) the fourth was perpendicular to the midpoint of the
third imaginary line. Then, the point where the first
imaginary line met the second imaginary line was
marked. This point was named as the meeting point. The
horizontal distance between the proximal tip and the
meeting point was measured as the width of the AF on
the coronal plane, and the vertical distance between the
distal tip and the meeting point was measured as the
length of the AF on the coronal plane (Fig. 2). Next, the
point where the fourth imaginary line intersected the AF
was marked. This point was named as the thickness
point, because we measured the thickness of the AF
from this point (Fig. 2). This measurement of thickness
was performed when the long axes of the jaws of the
digital calipers were parallel to the fourth imaginary line.
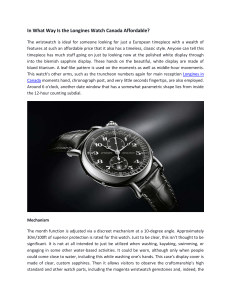
The vertical distance between the tip of the lateral
epicondyle of the humerus and the thickness point of the
AF was measured on the coronal plane and this distance
was named as the ‘‘distance AF’’ (Fig. 3). The vertical
distance between the tip of the lateral epicondyle of the
humerus and the tip of the styloid process of the radius
was measured as the ‘‘length of the forearm’’ on the
coronal plane (Fig. 3) to allow readers to understand the
size of the specimens and also to find the mean ‘‘ratio
AF’’. The ‘‘ratio AF’’ was found by dividing the distance
AF by the forearm length (ratio AF = distance AF/
Fig. 1. a Photograph of a
cadaver which has a tendinous
AF (right upper extremity).
bPhotograph of a cadaver
which has a membranous AF
(left upper extremity). rn, radial
nerve; bp, bifurcation point
(where the radial nerve divides
into its terminal branches); sb,
superficial branch of the radial
nerve; db, deep branch of the
radial nerve; AF, Arcade of
Frohse; sm, supinator muscle;
long arrow, proximal tip of the
AF; short arrow, distal tip of the
AF
172

forearm length) for each upper extremity. Then, the
mean value of the ratio AF was calculated. This value
may be used to predict the distance AF of any upper
extremity with a known forearm length. Thus, the pre-
dicted distance AF of any upper extremity may be found
by multiplying its forearm length by the mean ratio AF
(predicted distance AF = measured forearm length ·
mean ratio AF).
All the findings about the supinator muscle, the radial
nerve and its two terminal branches, and also the shape
and type of the AF, the appropriate measuring points
for each measurement and the accuracy of the mea-
surements were determined by the consensus of six
researchers.
Statistical analysis of all the measurements was per-
formed using the SPSS 7.5 statistical program (SPSS
Inc., Chicago, USA) for Windows, and the mean,
standard deviation and range of values were calculated
for each measurement.
The results of our study were compared with the
findings of previous studies.
Results
The supinator muscle, the radial nerve and its two ter-
minal branches showed no variations. In all the
extremities it was observed that the shape of the AF was
semicircular (Fig. 1a, b). In 87% of the extremities (48/
55) the AF was tendinous (Fig. 1a) and in 13% (7/55) it
was membranous (Fig. 1b). All our measurement results
are given as the mean±SD (minimum–maximum). The
width of the AF was 10.13±2.10 mm (5.65–13.61), the
length of the AF was 8.60±3.51 mm (2.77–20.20) and
the thickness of the AF was 0.77±0.34 mm (0.25–1.78).
The distance AF was 46.23±9.84 mm (24.97–84.04) and
the forearm length was 233.17±19.11 mm (196.23–
Fig. 2 Diagram of the width, length and thickness of the AF on the
photograph of a cadaver which has a tendinous AF (right upper
extremity). db, deep branch of the radial nerve; AF, Arcade of
Frohse; sm, supinator muscle; pt, proximal tip of the AF; dt, distal
tip of the AF; mp, meeting point (where the imaginary horizontal
line meets the imaginary vertical line); W, width of the AF (the
horizontal distance between the pt and the mp); L, length of the AF
(the vertical distance between the dt and the mp); tp, thickness point
(where the imaginary line perpendicular to the midpoint of the
imaginary line connecting the two tips of the AF intersects the AF).
The thickness of the AF was measured from the tp
Fig. 3 Diagram of the ‘‘distance AF’’ and the ‘‘forearm length’’
(left upper extremity). rn, radial nerve; db, deep branch of the radial
nerve; sb, superficial branch of the radial nerve; sm, supinator
muscle; AF, Arcade of Frohse; le, lateral epicondyle of the
humerus; sp, styloid process of the radius; D, ‘‘distance AF’’
(between the lateral epicondyle and the AF); L, ‘‘forearm length’’
(between the lateral epicondyle and the styloid process)
173

274.39). We found the ratio AF to be 0.199±0.047
(0.101–0.418). The mean ratio AF (=0.199) is approxi-
mately 1/5.
Discussion
The AF is most often reported as the site of the
compression of the DBRN in anatomical and clinical
studies [17]. The cause of compression of the DBRN at
the AF has been reported as only a tendinous AF [9,
26], or any pathological condition in addition to ten-
dinous AF [2,4] such as the space-occupying lesions
(ganglion, lipoma, etc.), edema, spasm, repeated rotary
movement, etc.
In 1908, Frohse and Fra
¨nkel [6] first described this
arch (AF) as a normal anatomical tendinous structure.
In his anatomical study of 25 adults and 10 full-term
fetuses, which was performed in 1968, Spinner [22] re-
ported that none of the newborn full-term fetuses had a
sharp tendinous AF, and that the most superior part of
the superficial layer of the supinator muscle was always
muscular. He suggested that the semicircular fibrous AF
probably formed in adults due to repeated rotary
movement of the forearm.
The percentage of tendinous AFs has varied from
30% to 80% in previous anatomical studies [4,5,13,14,
15,17,22,24,26]. The high percentages of tendinous
AFs were reported by Werner [26] (89%, 80/90 patients)
and by Lister et al. [10] (100%, 20/20 patients) in clinical
studies. In our study, the percentage of the tendinous
AFs was found to be 87%.
Debouck and Rooze [4] reported that the difference
between Spinner’s percentage of tendinous AFs (30%)
[22] and their own (64.1%) could be explained by a
difference in the classification criteria of the appearance
of the AF structure, or the fact that the two populations
were not comparable. They declared that the tendinous
AF was a normal anatomical structure.
According to Spinner [22], entrapment of the DBRN
becomes a distinct possibility when a tendinous AF is
present, particularly if it is thick, and the hiatus for the
passage of the nerve is narrow. In the light of Spinner’s
suggestion [22], we measured the width, length and
thickness of the AF. In the literature, the width, length
and thickness of the AF were measured only by Ebra-
heim et al. [5]. They found the width of the AF to be
2.8 mm, the length to be 18.6 mm and the thickness to
be 0.8 mm in male cadavers, and the width of the AF to
be 2.5 mm, the length to be 18.5 mm and the thickness
to be 0.7 mm in females.
The distance AF was reported as 3.8 cm by Low et al.
[11], 4.7 cm by Werner [26] and 4.91 cm by Papadopo-
ulos et al. [14]. However, they did not give any infor-
mation about forearm length. In our study, the distance
AF was found to be 46.23 mm.
The surgeon may calculate the predicted distance AF
of any upper extremity using our mean ratio AF, or may
easily find the predicted distance AF of any upper
extremity by dividing its forearm length by 5 (predicted
distance AF = forearm length of the patient/5).
Conclusions
The semicircular tendinous AF is anatomically a normal
condition in adult cadavers, but clinically it is a potential
anatomical factor causing compression of the DBRN.
Our measurements of the dimensions of the AF may
contribute to the anatomy of the AF. The mean ratio
AF may be used to localize the AF in this region during
forearm surgery. Awareness of the position of the AF
would assist the surgeon to better orientate during sur-
gery and thus reduce surgical complications. In partic-
ular, this ratio may be helpful for the surgeon whose
target is to decompress the DBRN in the surgical
treatment of the lateral elbow pain.
References
1. Arle JE, Zager EL (2000) Surgical treatment of common
entrapment neuropathies in the upper limbs. Muscle Nerve
23:1160–1174
2. Capener N (1966) The vulnerability of the posterior interos-
seous nerve of the forearm. A case report and an anatomical
study. J Bone Joint Surg Br 48:770–773
3. Cravens G, Kline DG (1990) Posterior interosseous nerve
palsies. Neurosurgery 27:397–402
4. Debouck C, Rooze M (1995) The arcade of Frohse: an ana-
tomic study. Surg Radiol Anat 17:245–248
5. Ebraheim NA, Jin F, Pulisetti D, et al (2000) Quantitative
anatomical study of the posterior interosseous nerve. Am
J Orthop 29:702–704
6. Frohse F, Fra
¨nkel M (1908) Die Muskeln des menschlichen
Armes. Fischer, Jena, pp 164–169
7. Fuss FK, Wurzl GH (1991) Radial nerve entrapment at the
elbow: surgical anatomy. J Hand Surg [Am] 16:742–747
8. Hashizume H, Nishida K, Nanba Y, et al (1996) Non-trau-
matic paralysis of the posterior interosseous nerve. J Bone Joint
Surg Br 78:771–776
9. Kopell HP, Thompson WAL (1963) Peripheral entrapment
neuropathies, 1st edn. William and Wilkins, Baltimore, pp 121–
128
10. Lister GD, Belsole RB, Kleinert HE (1979) The radial tunnel
syndrome. J Hand Surg [Am] 4:52–59
11. Low CK, Chew JTH, Mitra AK (1994) A surgical approach to
the posterior interosseous branch of the radial nerve through
the brachioradialis: a cadaveric study. Singapore Med J 35:394–
396
12. Moore KL, Dalley AF (1999) Clinically oriented anatomy, 4th
edn. Lippincott Williams and Wilkins, Philadelphia, pp 713,
730, 742, 746, 761
13. Ozkan M, Bacakoglu AK, Gul O, et al (1999) Anatomic study
of posterior interosseous nerve in the arcade of Frohse.
J Shoulder Elbow Surg 8:617–620
14. Papadopoulos N, Paraschos A, Pelekis P (1989) Anatomical
observations on the arcade of Frohse and other structures re-
lated to the deep radial nerve. Anatomical interpretation of
deep radial nerve entrapment neuropathy. Folia Morphol
(Praha) 37:319–327
15. Prasartritha T, Liupolvanish P, Rojanakit A (1993) A study of
the posterior interosseous nerve (PIN) and the radial tunnel in
30 Thai cadavers. J Hand Surg [Am] 18:107–112
16. Rath AM, Perez M, Mainguene C, et al (1993) Anatomic basis
of the physiopathology of the epicondylalgias: a study of the
deep branch of the radial nerve. Surg Radiol Anat 15:15–19
174

17. Riffaud L, Morandi X, Godey B, et al (1999) Anatomic bases
for the compression and neurolysis of the deep branch of the
radial nerve in the radial tunnel. Surg Radiol Anat 21:229–233
18. Ritts GD, Wood MB, Linscheid RL (1987) Radial tunnel
syndrome. A ten year surgical experience. Clin Orthop Relat
Res 219:201–205
19. Roles NC, Maudsley RH (1972) Radial tunnel syndrome:
resistant tennis elbow as a nerve entrapment. J Bone Joint Surg
Br 54:499–508
20. Rosenbaum R (1999) Disputed radial tunnel syndrome. Muscle
Nerve 22:960–967
21. Sotereanos DG, Varitimidis SE, Giannakopoulos PN, et al
(1999) Results of surgical treatment for radial tunnel syndrome.
J Hand Surg [Am] 24:566–570
22. Spinner M (1968) The arcade of Frohse and its relationship to
posterior interosseous nerve paralysis. J Bone Joint Surg Br
50:809–812
23. Sponseller PD, Engber WD (1983) Double-entrapment radial
tunnel syndrome. J Hand Surg [Am] 8:420–423
24. Thomas SJ, Yakin DE, Parry BR, et al (2000) The anatomical
relationship between the posterior interosseous nerve and the
supinator muscle. J Hand Surg [Am] 25:936–941
25. Verhaar J, Spaans F (1991) Radial tunnel syndrome. An
investigation of compression neuropathy as a possible cause.
J Bone Joint Surg Am 73:539–544
26. Werner CO (1979) Lateral elbow pain and posterior interos-
seous nerve entrapment. Acta Orthop Scand 174(Suppl):1–62
27. Williams PL, Bannister LH, Berry MM, et al (1995) Gray’s
anatomy, 38th edn. Churchill Livingstone, London, pp 851,
1273, 1274
175
1
/
5
100%