Guillain-Barré Syndrome Immunobiology: Anti-Ganglioside Antibodies
Telechargé par
clairedhoore

RICHARD P. BUNGE MEMORIAL LECTURE AND REVIEW
The immunobiology of Guillain-Barre
¤syndromes
Hugh J. Willison
Division of Clinical Neurosciences, Southern General Hospital, Glasgow, Scotland, UK
Abstract This presentation highlights aspects of the immunobiology of the Guillain-
Barre´ syndromes (GBS), the world’s leading cause of acute autoimmune neuromuscular
paralysis. Understanding the key pathophysiological pathways of GBS and developing
rational, specific immunotherapies are essential steps towards improving the clinical out-
come of this devastating disorder. Much of the research into GBS over the last decade has
focused on the forms mediated by anti-ganglioside antibodies, and we have made sub-
stantial progress in our understanding in several related areas. Particular highlights include
(a) the emerging correlations between anti-ganglioside antibodies and specific clinical
phenotypes, notably between anti-GM1/anti-GD1a antibodies and the acute motor axonal
variant and anti-GQ1b/anti-GT1a antibodies and the Miller Fisher syndrome; (b) the identi-
fication of molecular mimicry between GBS-associated Campylobacter jejuni oligosacchar-
ides and GM1, GD1a, and GT1a gangliosides as a mechanism for anti-ganglioside antibody
induction; (c) the development of rodent models of GBS with sensory ataxic or motor
phenotypes induced by immunisation with GD1b or GM1 gangliosides, respectively. Our
work has particularly studied the motor nerve terminal as a model site of injury, and
through combined active and passive immunisation paradigms, we have developed murine
neuropathy phenotypes mediated by anti-ganglioside antibodies. This has been achieved
through use of glycosyltransferase and complement regulator knock-out mice, both for
cloning anti-ganglioside antibodies and inducing disease. Through such studies, we have
proven a neuropathogenic role for murine anti-ganglioside antibodies and human GBS-
associated antisera and identified several determinants that influence disease expression
including (a) the level of immunological tolerance to microbial glycans that mimic self-
gangliosides; (b) the ganglioside density in target tissue; (c) the level of complement
activation and the neuroprotective effects of endogenous complement regulators; and
(d) the role of calcium influx through complement pores in mediating axonal injury. Such
studies provide us with clear information on an antibody-mediated pathogenesis model for
GBS and should lead to rational therapeutic testing of agents that are potentially suitable
for use in humans.
Key words: autoantibodies, Campylobacter jejuni, complement regulator, gangliosides,
glycosyltransferase, Guillain-Barre´ syndrome, membrane attack complex, neuromuscular
synapse, neuropathy, tolerance
Introduction
Autoimmune neuropathies are a diverse group of
paralytic syndromes characterised by inflammation in
the peripheral nervous system (PNS), in turn initiated by
a range of quite distinct immunopathological
events. Understanding the immunological mechanisms
Address correspondence to: Prof. Hugh J. Willison, Division of
Clinical Neurosciences, Institute of Neurological Sciences, Southern
General Hospital, Glasgow G51 4TF, Scotland, UK. Tel: þ44-141-201-
2464; Fax: þ44-141-201-2993; E-mail: [email protected]
Journal of the Peripheral Nervous System 10:94–112 (2005)
2005 Peripheral Nerve Society 94 Blackwell Publishing

underlying any pathological responses is clearly crucial to
selecting the correct strategies for novel therapeutic inter-
ventions, and this is particularly germane to the Guillain-
Barre´ syndromes (GBS) where the relative involvement of
T- and B-cell responses is continually debated. In recent
years, great progress has been made in our understand-
ing of this group of disorders. Out of many avenues
explored, one of the most promising has been the dis-
covery and analysis of antibody responses to peripheral
nerve gangliosides and their microbial mimics, the rela-
tionships these have to different clinical phenotypes of
GBS, and our increasing insights into their mechanisms of
action. Despite this rapidly advancing progress, consider-
able gaps in our knowledge persist. The focus of this
lecture is on gangliosides and their corresponding auto-
antibodies in GBS. I will first provide a brief background to
the field, summarise some of the highlights, identify and
analyse areas of remaining weakness, and then present
some data to support novel therapeutic approaches that
could capitalise on the latest experimental findings.
The Clinical Problem
GBS is the prototypic acute inflammatory disorder
and the foremost cause of post-infectious neuromuscu-
lar paralysis worldwide, with a global incidence of
approximately 1.5/10
5
across all age groups (Hughes
and Rees, 1997; Hahn, 1998). The lifetime likelihood of
any one individual acquiring the disease is thus approxi-
mately 1 : 1000. Onset is rapid, and approximately 20%
of cases lead to total paralysis, requiring prolonged
intensive therapy with mechanical ventilation. The ther-
apeutic window for GBS is short, and the current opti-
mal treatment with whole plasma exchange or
intravenous immunoglobulin (Ig) therapy lacks immuno-
logical specificity and only halves the severity of the
disease (Visser et al., 1999; 2004; Raphael et al., 2001;
Hughes et al., 2004a; 2004b). The patients left severely
disabled (approximately 12% survivors unable to walk
after 1 year) or dead (UK mortality of 5–10%) represent
a major social and economic burden (Buzby et al., 1997).
Thus, there is an incentive to understand GBS patho-
genesis as a prerequisite to developing and instituting
effective, contemporary immunotherapies.
Clinical and Pathological Patterns of GBS
Despite the all-embracing eponym, GBS’s clinical
pathophysiology is long recognised as being highly com-
plex (Hartung et al., 1995a; 1995b). GBS is an acute
phase illness occurring 10–14 days after trivial infections,
comes and goes rapidly (within 4 weeks), and leaves
variable residual injury. The acute, monophasic nature
of GBS provides crucial clues to the immunopathological
background and quite clearly distinguishes GBS from
most other pro-inflammatory insults that lead to neuro-
pathy. The commonest form of GBS arises from seg-
mental demyelination of peripheral nerve (acute
inflammatory demyelinating polyneuropathy [AIDP]),
executed by macrophage-mediated stripping of the mye-
lin sheath (Hafer-Macko et al., 1996b). At least a propor-
tion of this injury appears to be mediated by antibody and
complement deposition on Schwann cell and myelin
membranes, although the putative antigenic target(s) in
AIDP remain elusive, as discussed below. Clinically, this
demyelinating process is widespread, affecting most
myelinated limb, axial and lower cranial motor and sen-
sory nerves, but curiously sparing myelinating axons
innervating extraocular muscles that are so sensitively
affected in Miller Fisher syndrome (MFS). Resting intra-
neural Schwann cells proliferate and migrate into the
lesion sites to remyelinate denuded axons, producing a
good recovery in most cases. In AIDP, demyelinating
pathology may be extensive throughout the length of
the nerve, especially in proximal nerve roots and the
distal intramuscular nerve segments where the blood–
nerve barrier (BNB) is weak (Olsson, 1968).Inagree-
ment, clinical electrophysiological studies indicate that
sites throughout the nerve can be affected but often
point towards proximal (absent or delayed F-wave laten-
cies) or distal (prolonged distal motor latencies) as domi-
nant sites of nerve impairment. It would seem intuitively
likely that the rate of recovery from AIDP should be
independent of the site of demyelination because there
is no evidence that the remyelinating capacity of
Schwann cells varies along the length of the nerve.
Axons are generally unaffected in AIDP, although may
suffer so-called bystander injury, the mechanisms for
which remain unclear and deserve further study.
In contrast to AIDP, the primary target for immune
attack in the GBS variant, acute motor (and sensory)
axonal neuropathy (AMAN, AMSAN) is the axolemmal
membrane (Feasby et al., 1986; McKhann et al., 1993).
Again, this inflammatory process occurs predominantly
either in the nerve roots or distal nerve terminals
(Hafer-Macko et al., 1996a; Ho et al., 1997a;
Kuwabara et al., 2003). Immune attack can lead to
reversible axonal conduction block due to reversible
axonal injury (at best) or complete axonal transaction
(at worst). Wallerian degeneration (Wld) will occur dis-
tal to the site if axons are transected; otherwise, mye-
lin is unaffected. Depending on the site of transection
(proximal or distal), axonal recovery may be poor or
good, owing to the distance over which regeneration
is effective (Ho et al., 1997a; 1997b). This is important
clinically because extensive radicular involvement in
AMAN generally leads to a catastrophic, permanent
injury. In contrast, very distal axonal injury would also
induce a severe acute axonal syndrome, but one in
which rapid reinnervation with functional recovery
Willison Journal of the Peripheral Nervous System 10:94–112 (2005)
95

could readily occur (Ho et al., 1997a; Kuwabara et al.,
2003).
Formes Frustes of GBS Also Exist as
Regional Variants
The regional variants of GBS only paralyse specific
areas of the body, such as the eyes or face, or the
afferent sensory and autonomic systems (Ropper,
1994). The most widely studied of these variants is the
MFS (Fisher, 1956; Willison and O’Hanlon, 1999).Our
understanding of MFS was revolutionised following
Chiba and Kusunoki’s discovery of the anti-GQ1b anti-
body marker (Chiba et al., 1992; 1993). Since the syn-
drome was first described in 1956 as the discrete clinical
triad of ophthalmoplegia, ataxia, and areflexia, anti-GQ1b
antibody testing has allowed MFS to evolve nosologi-
cally and now encompasses closely related formes
frustes, mainly characterised by acute cranial motor neu-
ropathies with ataxia – the anti-GQ1b antibody syn-
dromes (Odaka et al., 2001; Paparounas, 2004).Inthe
Bickerstaff’s encephalitis, MFS-like features occur in
conjunction with brain stem involvement, comprising
pyramidal tract signs and impaired consciousness, and
two thirds of cases are anti-GQ1b antibody positive
(Bickerstaff and Cloake, 1951; Odaka et al., 2003).The
close relationship between GBS and MFS is considered
because it should direct our search towards common
underlying immunopathological mechanisms. Thus,
some MFS cases merge into confluent GBS with
respiratory and limb involvement, and similarly, some
GBS cases also evolve to develop an MFS pattern of
clinical involvement – in these overlapping cases, anti-
GQ1b antibodies are generally detected. MFS variants
include solitary ophthalmoplegia or ataxia and orophar-
yngeal weakness without ophthalmoplegia (O’Leary
et al., 1996). Viewed in its broadest contemporary
sense, MFS could be considered as a PNS/CNS overlap
syndrome with extremely variable degrees of involve-
ment of particular central or peripheral anatomical sites
in individual cases, with all permutations being highly
associated with anti-GQ1b and anti-GT1a antibodies
(O’Leary et al., 1996; Odaka et al., 2001).
The selective affliction of cranial and in particular
extraocular nerves in the anti-GQ1b antibody syn-
dromes is believed to be due to the enrichment of
the target antigen(s) in affected sites (Chiba et al.,
1997). However, there are clearly additional levels of
complexity influencing the clinical phenotype that
remain undiscovered. What is notable by its absence
is involvement of extraocular motor nerves in AIDP,
arguing that the AIDP antigen(s) may analogously be
relatively enriched in limb and axial myelin (in compar-
ison with extraocular motor nerve myelin) as opposed
to being a generic myelin antigen(s). This might
mitigate against the major structural proteins of myelin
being dominant AIDP antigens. A chronic ataxic neuro-
pathy has also been reported that may be associated
with relapsing ophthalmoplegia in some cases; such
patients often have anti-ganglioside antibodies, includ-
ing anti-GQ1b, which are persistently present, usually
occurring as IgM paraproteins (Willison et al., 2001).
Anti-Nerve Antibodies in GBS: Lessons
From Rodent Models
Great progress has been made in correlating clinical
phenotypes with serological profiling of anti-nerve antibo-
dies, covering a wide spectrum of peripheral nerve anti-
gens. The myelin protein-specific T and B cell-mediated
rodent model of GBS (experimental allergic neuritis [EAN])
was described 50 years ago and has yielded many impor-
tant experimental insights into peripheral nerve inflamma-
tion (Spies et al., 1995; Rostami, 1997; Gabriel et al., 1998;
Taylor and Pollard, 2003). However, translational studies
identifying equivalent immune responses in human neuro-
pathy cases have been more modest (Gabriel et al., 2000;
Ritz et al., 2000; Yan et al., 2000; Favereaux et al., 2003;
Latov and Renaud, 2004). Whether further research will
overcome this remains to be seen.
In contrast, the progress in identifying myelin and
axonal glycolipids as antigens has been somewhat
more forthcoming. Interestly that ganglioside-/glycolipid-
induced rabbit EAN was also first described several
decades ago (Nagai et al., 1976; Saida et al., 1979),
but in contrast to myelin protein-induced EAN, was
then virtually neglected for approximately 20 years,
and has now been revived with compelling data that
reinforce many recent clinical findings. Thus, a series
of recent rabbit immunisation studies have led to the
generation of models of anti-GD1b antibody-associated
ataxic neuropathy and anti-GM1 antibody-associated
motor axonal neuropathy that mimic many of the clin-
ical and pathological features of the human syndromes
(Kusunoki et al., 1996; Yuki et al., 2001; 2004).
These studies have provided some of the most
compelling evidence that anti-ganglioside antibodies
and their effector pathways can induce clinically rele-
vant phenotypes. In this respect, ganglioside-induced
EAN has come full circle. The return of researchers,
principally in Japan, to these early rabbit studies was
driven in large part by the clinical identification of anti-
ganglioside antibodies in GBS cases, starting in 1988
(Ilyas et al., 1988) and escalating in scope ever since. A
wealth of clinical serological associations have now been
described and the topic reviewed regularly (Yuki, 2001;
Willison and Yuki, 2002). In summary, in human disease,
anti-GM1, anti-GD1a, anti-GM1b, and anti-GalNAcGD1a
antibodies are highly associated with AMAN (Ogawara
et al., 2000) and anti-GQ1b, anti-GT1a, anti-GD3, and
Willison Journal of the Peripheral Nervous System 10:94–112 (2005)
96

anti-GD1b with MFS and chronic ataxic neuropathy
(Chiba et al., 1993; Willison et al., 2001). Anti-GM1 IgG/
IgM antibodies are also associated with AIDP and
chronic demyelinating clinical phenotypes, the latter
with or without concomitant axonopathy, as seen in
multifocal motor neuropathy (Pestronk and Choksi,
1997). However, considerable debate still remains as to
the relative extent of demyelinating and axonal pathol-
ogy that can be associated with anti-GM1 antibody syn-
dromes. An exciting new finding has suggested that
gangliosides assembled in complexes (in this case
GM1 and GD1a) (Kaida et al., 2004) might provide higher
avidity targets for GBS-associated autoantibodies than
single ganglioside species. Although it has long been
known that accessory lipids play an important role in
enhancing or attenuating ganglioside–antibody interac-
tions, this provocative finding greatly raises the complex-
ity of examining sera for the new autoantibody
specificities, including the elusive AIDP antigen(s).
Gangliosides and Structural Mimics on
Microbial Glycans
One highly fruitful area has been the discovery of a
range of ganglioside and glycolipid mimics on microbial
glycans (Yuki et al., 1993; Yuki, 2001). There are
approximately 50 structurally distinct gangliosides
synthesised through step-wise addition of monosac-
charides by Golgi glycosyltransferases in complex
developmental, spatial, and cell-specific patterns
(Kolter et al., 2002). Gangliosides are enriched in neural
tissues and primarily localised to raft domains of the
extracellular leaflet of plasma membranes, especially
at synapses, where they are available for anti-
ganglioside antibody binding (Ledeen, 1978; Ledeen and
Yu, 1982; Ledeen et al., 1998; Ogawa-Goto and Abe,
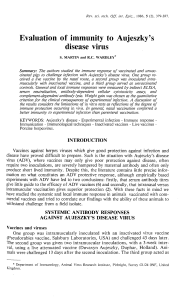
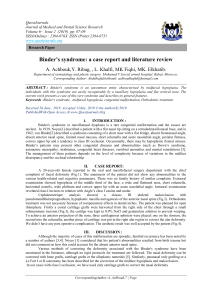
1998). A simplified scheme of the major ganglioside
structures is shown in Figure 1. The carbohydrate moi-
eties of gangliosides are structural mimics of microbial
glycans, including the lipo-oligosaccharides (LOS) of
Campylobacter jejuni (Aspinall et al., 1994; Yuki et al.,
1997; Sheikh et al., 1998; Prendergast and Moran,
2000; Moran et al., 2002) and Haemophilus influenzae
(Mori et al., 1999; Ju et al., 2004). Evidence from
human and animal studies indicates a key role for this
molecular mimicry in GBS pathogenesis (Goodyear
et al., 1999; Bowes et al., 2002; Yuki et al., 2004).In
this model, well documented for GM1, GD1a, and
GQ1b, the acute phase anti-LOS/ganglioside complement-
fixing IgG antibodies that arise eradicate infections but
also bind to peripheral nerve gangliosides where they
induce autoimmune injury. Potential pathogenic role(s)
exist for other known and unknown glycolipids
enriched in Schwann cell, myelin, and axonal mem-
branes, such as galactocerebroside, LM1, and
sulfatides that also have microbial glycan mimics
(Yuki, 2001; Willison and Yuki, 2002).
Immunological Tolerance Exists to
Self-Ganglioside Structures
One of the curiosities of GBS is that such a small
proportion of infections or vaccinations triggers the
illness. Thus, 99% of humans infected with ganglio-
side-mimicking strains of C. jejuni neither develop anti-
LOS/ganglioside antibodies nor GBS (Nachamkin,
2001). The immunological factors that regulate this
unresponsiveness to challenge with microbial mimics
of self-glycan structures are poorly understood, but
it seems likely that B-cell tolerance is an important
component. Anti-LOS/ganglioside antibodies exist
within the natural antibody repertoire, acting as
innate defence against bacteria. Being carbohydrates,
gangliosides elicit T cell-independent (TI) humoral
responses (Martin et al., 2001; Zubler, 2001) and can-
not be presented by major histocompatibility complex
molecules (Ishioka et al., 1993) (except via CD1 pre-
sentation [Brigl and Brenner, 2004; Watts, 2004] ).
Anti-ganglioside antibodies exist as low-affinity IgM
isotypes in normal subjects (Willison et al., 1993;
Mizutamari et al., 1994; Casali and Schettino, 1996).
To prevent autoimmune reactions, their level and affi-
nity are controlled by tolerance (Cornall et al., 1995;
Fagarasan and Honjo, 2000). In GBS, the appearance
of high titre anti-ganglioside antibodies is a clear failure
of tolerance. B-cell tolerance to TI ganglioside antigens
is poorly understood and remains a major research
goal in the GBS field. Aspects are analogous to organ
transplantation paradigms involving Gal(a1–3)Gal anti-
gens as studied in a1–3galactosyltransferase knock-
out (KO) mice (Kawahara et al., 2003; Galili, 2004)
and in the ABO blood group system (Fan et al., 2004;
Fehr and Sykes, 2004).
We and others anticipated that the expression of
gangliosides in tissues outside the nervous system
that can be sensed by newly developing and pre-exist-
ing B cells (bone marrow and spleen, respectively)
would be an important regulator of tolerance, as sug-
gested for anti-Gal(a1–3)Gal (Yang et al., 1998). Thus,
we showed that mice lacking complex gangliosides in
any tissue (i.e., the GalNAcT KO mice that only
express GM3 and GD3, see Fig. 1) develop exagger-
ated humoral responses to gangliosides compared
with wild-type (WT) controls when challenged with
C. jejuni LOS (Bowes et al., 2002) or gangliosides
(Lunn et al., 2000). An example of the differential anti-
body responses to GD1a ganglioside and GD1a-bearing
C. jejuni LOS in GalNAcT WT and KO mice that clearly
illustrates this principle is shown in Figure 2.
Willison Journal of the Peripheral Nervous System 10:94–112 (2005)
97

Isolating and Characterising Murine
Monoclonal Anti-Ganglioside Antibodies
An offshoot of these experiments aimed at
bypassing tolerance to microbial glycans has been
the creation of high-affinity IgG responses to ganglio-
sides that are suitable for cloning top quality anti-gang-
lioside antibodies – a long-awaited goal for these
poorly immunogenic structures. In addition to over-
coming any tolerogenic factors, to circumvent any TI
restriction on affinity maturation and class switching
(including that which might occur in glycosyltransferase
KO mice), we have developed hapten-carrier
immunisation protocols using ganglioside–protein
conjugates and LOS/ganglioside liposome-encapsulated
proteins to provide the necessary T cell-dependent
(TD) environment required to produce the magnitude
of immune responses seen in Figure 2. Using these
methods, we and others have generated long-lived IgG
memory responses to gangliosides and to LOS in gly-
cosyltransferase KO mice. Using such an approach,
we have cloned approximately 50 IgG/IgM monoclonal
antibodies specific for discrete ganglioside epitopes for
use in a wide range of pathogenesis and therapeutic
studies (Boffey et al., 2004; Willison et al., 2004).
Ugcg–/– Cer
Cer
Cer
Cer
Cer
GA2
A simplified scheme of the ganglioside biosynthetic pathway
Cer
GA1
Cer
GM1b
Cer 0 series
a series
b series
GD1c
Cer
GT1a
Cer
GQ1b
Cer
GD1a
Cer
GT1b
Cer
GM1a
Cer
GD1b
Cer
GM2
Cer
GD2
GM1
HS:19(GM1+, GD1a+) and HS:4 HS:19(GM1+, GT1a+)
Lipid A
Galactose Glucose NeuNAc Cer Ceramide
GalNAc
Key
Lipid A Lipid A Lipid A Lipid A
HS:10
Examples of Campylobacter jejuni LOS stuctures
Candidate oligosaccharide fragments for inhibition/immunoadsorption studies
GD1a GQ1b
Cer
GlcCer
A
B
C
LacCer
GD3s–/–
GM3
GD3
GalNAcT–/–
Figure 1. A schematic representation of the key structures and enzymes in ganglioside biosynthesis, relevant glycan
fragments, and core structures identified in Campylobacter jejuni lipo-oligosaccharides. Note that GalNAc transferase
(GalNAcT) and GD3 synthase (GD3s) deficiency result in the loss of all complex and b-series gangliosides, respectively.
Willison Journal of the Peripheral Nervous System 10:94–112 (2005)
98
 6
6
 7
7
 8
8
 9
9
 10
10
 11
11
 12
12
 13
13
 14
14
 15
15
 16
16
 17
17
 18
18
 19
19
1
/
19
100%



![[msg.mbi.ufl.edu]](http://s1.studylibfr.com/store/data/009538701_1-491901e69c929a148945022b9b4a9fe7-300x300.png)
