Cardiac Surgery Site Infections: Epidemiology & Prevention
Telechargé par
rabiakhouildi

Please
cite
this
article
in
press
as:
Lepelletier
D,
et
al.
Epidemiology
and
prevention
of
surgical
site
infections
after
cardiac
surgery.
Med
Mal
Infect
(2013),
http://dx.doi.org/10.1016/j.medmal.2013.07.003
ARTICLE IN PRESS
+Model
MEDMAL-3432;
No.
of
Pages
7
Disponible
en
ligne
sur
www.sciencedirect.com
Médecine
et
maladies
infectieuses
xxx
(2013)
xxx–xxx
General
review
Epidemiology
and
prevention
of
surgical
site
infections
after
cardiac
surgery
Épidémiologie
et
prévention
des
infections
du
site
opératoire
après
chirurgie
cardiaque
D.
Lepelletier a,∗,d,
C.
Bourigault a,
J.C.
Roussel b,
C.
Lasserre a,
B.
Leclère a,
S.
Corvec a,d,
S.
Pattier b,
T.
Lepoivre e,
O.
Baron b,c,
P.
Despins b,c
aService
de
bactériologie
et
d’hygiène
hospitalière,
unité
de
gestion
du
risque
infectieux,
CHU
de
Nantes,
bâtiment
Le
Tourville,
5,
rue
du
Pr-Yves-Boquien,
44093
Nantes
cedex
01,
France
bService
de
chirurgie
thoracique
et
cardiovasculaire,
CHU
de
Nantes,
44000
Nantes,
France
cInserm
UMR
S
1087,
université
de
Nantes,
institut
du
thorax,
44000
Nantes,
France
dUFR
médecine,
université
de
Nantes,
EA
3826,
Nantes,
France
eDépartement
d’anesthésie-réanimation,
44000
Nantes,
France
Received
14
September
2012;
received
in
revised
form
20
June
2013;
accepted
19
July
2013
Abstract
Deep
sternal
wound
infection
is
the
major
infectious
complication
in
patients
undergoing
cardiac
surgery,
associated
with
a
high
morbidity
and
mortality
rate,
and
a
longer
hospital
stay.
The
most
common
causative
pathogen
involved
is
Staphylococcus
spp.
The
management
of
post
sternotomy
mediastinitis
associates
surgical
revision
and
antimicrobial
therapy
with
bactericidal
activity
in
blood,
soft
tissues,
and
the
sternum.
The
pre-,
per-,
and
postoperative
prevention
strategies
associate
controlling
the
patient’s
risk
factors
(diabetes,
obesity,
respiratory
insufficiency),
preparing
the
patient’s
skin
(body
hair,
preoperative
showering,
operating
site
antiseptic
treatment),
antimicrobial
prophylaxis,
environmental
control
of
the
operating
room
and
medical
devices,
indications
and
adequacy
of
surgical
techniques.
Recently
published
scientific
data
prove
the
significant
impact
of
decolonization
in
patients
carrying
nasal
Staphylococcus
aureus,
on
surgical
site
infection
rate,
after
cardiac
surgery.
©
2013
Elsevier
Masson
SAS.
All
rights
reserved.
Keywords:
Cardiac
surgery;
Surgical
site
infection;
Risk
factors;
Prevention
Résumé
Les
infections
du
site
opératoires
profondes
représentent
la
complication
infectieuse
majeure
de
la
chirurgie
cardiaque.
Essentiellement
staphy-
lococciques,
elles
nécessitent
une
reprise
chirurgicale
précoce
et
une
antibiothérapie
rapidement
bactéricide
au
niveau
du
sang,
des
tissus
mous
et
du
sternum.
Leurs
conséquences
sont
sévères
en
termes
de
morbidité
et
d’allongement
de
la
durée
de
séjour
hospitalier.
Les
stratégies
de
prévention
pré,
per-
et
postopératoire
associent
le
contrôle
des
facteurs
liés
aux
patients
(obésité,
diabète,
insuffisance
respiratoire),
la
préparation
cutanée
corporelle
(traitement
des
pilosités,
douche
préopératoire,
antisepsie
du
site
opératoire),
l’antibioprophylaxie,
la
maîtrise
de
l’environnement
du
bloc
opératoire
et
des
dispositifs
médicaux
mais
aussi
les
indications
et
la
qualité
des
techniques
opératoires.
Les
données
récentes
de
la
littérature
scientifique
montrent
un
impact
significatif
de
la
décolonisation
des
patients
porteurs
de
staphylocoques
doré
au
niveau
nasal
sur
le
taux
d’infection
du
site
opératoire
après
chirurgie
cardiaque.
©
2013
Elsevier
Masson
SAS.
Tous
droits
réservés.
Mots
clés
:
Chirurgie
cardiaque
;
Infection
du
site
opératoire
;
Facteurs
de
risque
;
Prévention
∗Corresponding
author.
E-mail
address:
didier[email protected]
(D.
Lepelletier).
1.
Introduction
More
than
40,000
cardiac
surgery
procedures
are
performed
every
year
in
France.
Deep
sternal
wound
infection
(mediastini-
tis)
is
the
most
severe
complication
and
surgical
site
infection
0399-077X/$
–
see
front
matter
©
2013
Elsevier
Masson
SAS.
All
rights
reserved.
http://dx.doi.org/10.1016/j.medmal.2013.07.003

Please
cite
this
article
in
press
as:
Lepelletier
D,
et
al.
Epidemiology
and
prevention
of
surgical
site
infections
after
cardiac
surgery.
Med
Mal
Infect
(2013),
http://dx.doi.org/10.1016/j.medmal.2013.07.003
ARTICLE IN PRESS
+Model
MEDMAL-3432;
No.
of
Pages
7
2
D.
Lepelletier
et
al.
/
Médecine
et
maladies
infectieuses
xxx
(2013)
xxx–xxx
(SSI)
in
cardiac
surgery
performed
mainly
by
median
ster-
notomy
[1].
Its
incidence
is
relatively
low
and
has
remained
for
several
years,
but
it
concerns
4000
to
8000
increasingly
fragile
patients
every
year,
whose
risk
of
mortality
is
increased
from
10
to
40%
[2–4].
All
cardiac
surgery
units
in
France
are
concerned
by
the
occurrence
of
mediastinitis
and
confronted
to
its
severity
at
short
or
long
term,
to
its
difficult
management,
and
to
significant
over-cost
[5].
The
surgical
teams
in
these
units
have
developed
SSI
prevention
strategies
in
collaboration
with
hygienists,
anesthesiologists,
and
critical
care
specialists,
based
on
recent
recommendations,
particularly
those
concerning
antibiotic
prophylaxis
[6]
and
patient
preparation
[7].
Besides
these
recommendations,
choosing
preventive
measures
relies
on
the
knowledge
and
management
of
risk
factors
related
to
patients,
to
the
surgery,
and
to
the
operating
room
environment
[8].
The
prognosis
depends
on
the
delay
before
diagnosis
and
treatment,
on
the
therapeutic
method,
and
on
the
effectiveness
of
antibiotherapy.
The
definition,
the
incidence,
and
the
risk
fac-
tors
for
SSI
after
cardiac
surgery
are
presented
in
this
review.
We
have
summarized
the
main
strategic
orientations
currently
recommended
for
the
prevention
of
these
sometimes
devastating
infectious
complications.
2.
Definition
and
classification
of
surgical
site
infection
after
cardiac
surgery
SSI
include
superficial
infections
of
the
postoperative
scar
and
deep
wound
infections
such
as
sternal
osteitis,
mediastini-
tis,
and
endocarditis.
The
definitions
of
postoperative
SSI
are
adapted
from
those
issued
by
the
National
Technical
Committee
on
Nosocomial
Infections
and
Care
Related
Infections
(French
acronym
CTINILS
2007)
[9],
which
had
been
adapted
from
those
issued
by
the
centers
for
disease
control
and
prevention
(CDC)
[10].
2.1.
Superficial
wound
infections
Superficial
wound
infections
concern
the
skin
and
subcuta-
neous
tissue.
The
signs
(redness,
fluid
collection,
disunion)
are
always
local.
The
sternum
is
not
involved,
stable,
and
painless
on
bi-manual
palpation.
Most
of
the
time,
it
requires
only
local
(disinfection,
warm
pads)
and
oral
(antibiotics)
treatment.
But
it
may
extend
to
deeper
layers
at
any
time.
2.2.
Deep
infection
Deep
infection
includes
the
previously
mentioned
lesions
and
is
defined
by
the
involvement
of
tissue
below
the
subcutaneous
layer
with
at
least
one
of
the
following
criteria:
•
positive
culture
of
tissue
samples
or
mediastinal
fluid;
•
typical
presentation
of
mediastinitis
on
revision
surgery
or
anatomopathological
examination;
•
presence
of
one
of
the
following
elements:
fever
superior
to
38 ◦C,
thoracic
pain
or
sternal
instability,
with
either
pus
in
the
mediastinum,
or
positive
culture
of
peroperative
samples
or
of
hemoculture
(or
both
in
case
of
germs
commensal
of
the
cutaneous
flora).
Only
surgical
exploration
can
document
the
true
nature,
the
extent,
and
the
prognosis
of
infection.
Despite
the
helpfulness
of
these
definitions,
the
use
of
dif-
ferent
terms
to
define
SSI
may
account
for
the
difficulty
to
clearly
define
and
measure
its
incidence
[11].
Sternal
wound
complications
range
from
sterile
dehiscence
to
suppurative
mediastinitis,
and
the
terms
of
sternitis
or
sternal
osteitis
(surgi-
cal
revision
without
sternal
opening)
and
mediastinitis
(surgical
revision
with
sternal
opening)
are
used
to
define
deep
infection.
Some
definitions
published
in
the
2000s
are
author
specific
such
as
El
Oakley’s
or
Gardlund’s
[12,13].
Furthermore,
the
repro-
ducibility
of
SSI
diagnosis
may
vary
according
to
the
depth
of
infection
[11,14];
the
medical
specialty
of
the
physician
also
has
an
impact
(surgeon,
anesthesiologist,
infectious
dis-
ease
specialist,
bacteriologist,
hygienist),
stressing
the
need
for
a
multidisciplinary
approach
[14].
3.
Incidence
of
surgical
site
infection
in
cardiac
surgery
The
rate
of
SSI
varies
according
to
the
quality
of
the
local
epidemiological
surveillance
[15]
or
of
surveillance
networks,
of
the
SSI
definition
used
(superficial,
deep),
of
the
patient’s
profile,
and
of
the
type
surgical
procedure
[16,17].
The
true
global
incidence
of
infection
in
cardiac
surgery
is
thus
difficult
to
assess.
In
France,
the
alert,
investigation,
and
surveillance
of
nosocomial
infections
(French
acronym
RAISIN)
network
data
concerning
cardiac
surgery
is
made
on
too
small
samples
to
be
representative
[16].
According
to
some
authors
and
to
simplify
data
collection,
the
surveillance
of
patients
reviewed
surgically
(with
or
without
sternal
re-opening)
from
the
operating
room
and
onward,
would
allow
measuring
reliably
and
easily
the
incidence
of
deep
SSI
[3].
The
incidence
of
mediastinitis
after
the
1990s
has
not
decreased
compared
to
the
1970–1980s,
ranging
between
0.5%
and
4.4%
[18].
Various
scores
have
been
built
and
used
to
stratify
the
incidence
of
postoperative
SSI
according
to
risk
fac-
tors.
The
American
score
of
the
National
Nosocomial
Infections
Surveillance
(NNIS)
System
integrates
the
ASA
physical
status
score,
the
Altemeier
contamination
classification,
and
the
length
of
surgery
[19].
Other
scores
have
been
proposed
for
predic-
tion
based
on
factors
more
specifically
associated
to
the
risk
of
mediastinitis
identified
by
comparatives
studies
in
multivariate
analysis
[20–22].
4.
Physiopathology
of
surgical
site
infection
after
cardiac
surgery
The
contamination
of
the
operative
site
may
be
due
to
the
patient’s
endogenous
flora
or
to
the
surgical
team’s
or
operating
room
exogenous
flora,
and
is
often
peri-operative.
Some
factors
promote
the
occurrence
of
SSI
from
this
contamination,
such
as
tissue
necrosis,
hematoma,
foreign
body,
of
a
prosthesis
or
of
an
implant,
and
bad
vascularization.

Please
cite
this
article
in
press
as:
Lepelletier
D,
et
al.
Epidemiology
and
prevention
of
surgical
site
infections
after
cardiac
surgery.
Med
Mal
Infect
(2013),
http://dx.doi.org/10.1016/j.medmal.2013.07.003
ARTICLE IN PRESS
+Model
MEDMAL-3432;
No.
of
Pages
7
D.
Lepelletier
et
al.
/
Médecine
et
maladies
infectieuses
xxx
(2013)
xxx–xxx
3
4.1.
The
impact
of
endogenous
flora
The
impact
of
endogenous
flora
is
essential
in
the
phys-
iopathology
of
SSI.
Since
the
late
1990s
it
was
acknowledged
that
nasal
colonization
by
Staphylococcus
aureus
was
a
risk
fac-
tor
for
S.
aureus
SSI
after
cardiac
surgery
[23,24]
with
a
great
similitude
of
colonization
and
infection
strains.
4.2.
The
exogenous
contamination
The
exogenous
contamination
of
the
operative
site
is
either
handborne
or
airborne.
The
airborne
contamination
requires
two
associated
phenomena,
the
presence
of
microorganisms
(air
bio-
contamination)
and
of
inert
particles
(air
contamination)
some
of
which
are
used
as
support
by
bacteria.
The
microorganisms
often
come
from
the
usual
saprophyte
flora
of
air
(rarely
pathogenic)
and
from
the
commensal
human
flora
(mostly
S.
aureus,
coagu-
lase
negative
staphylococci,
sometimes
Gram-negative
bacteria)
released
by
human
bodies
(patients
and
surgical
team)
[8,25].
The
particles
are
released
by
individuals
(cutaneous
squamous
cells,
skin
appendages,
respiratory
droplets,
and
droplet
nuclei),
and
textiles
(surgical
team’s
clothes
and
operative
field
drapes);
the
quantity
is
proportional
to
the
number
of
individuals
present
in
the
room
and
to
their
movements
and
moving
around,
as
well
as
to
the
quality
of
textiles
used
(no-woven
and
polycoton
drapes
emit
less
particles
than
cotton
drapes
and
more
parti-
cle
proof)
[26].
The
surgical
team’s
flora
is
rarely
the
cause.
Contamination
by
soiled
material,
very
rare,
has
now
become
exceptionally
rare
because
of
the
recent
strengthening
of
steril-
ization
and
disinfection
guidelines
for
materials,
and
the
use
of
disposable
sterile
material.
Other
rare
modes
of
postoperative
contamination
may
be
mentioned,
particularly
hematogenous
ones
from
an
infection
occurring
in
postoperative
critical
care
(catheter
bacteremias
[27]
or
pneumonia)
or
by
direct
bacterial
inoculation
of
the
operative
site
when
changing
wound
dressing
in
patients
presenting
with
scarring
abnormalities.
Three
major
hypotheses
can
be
considered
concerning
the
chronology.
The
infection
is
localized
after
contamination,
responsible
second-
arily
for
localized
sternal
osteomyelitis,
inducing
the
disunion
of
fasciae.
Other
authors
believe
there
is
first
a
separation
of
sternal
margins
leading
to
the
disunion
of
fasciae
secondarily
colonized
by
bacteria.
The
last
admitted
hypothesis
is
that
of
the
poor
drainage,
with
a
large
stagnant
collection,
favoring
bacterial
development
[28].
5.
Microbiology
Staphylococci
are
the
main
bacteria
responsible
for
post-
operative
SSI,
even
if
their
proportion
may
vary
according
to
reports.
S.
aureus
accounts
for
40
to
60%
of
strains
causing
mediastinitis.
Coagulase
negative
staphylococci
are
involved
in
20
to
30%
of
cases
(Table
1).
20
to
30%
of
mediastinitis
cases
are
caused
by
Gram-negative
bacilli
and
rarely
by
yeasts
[28].
Some
authors
have
described
various
types
and
times
of
bacte-
rial
contamination
(pre-,
per-,
and
postoperative)
according
to
microbiological
documentation
[13].
Table
1
Microbiological
documentation
of
mediastinitis
after
cardiac
surgery.
Documentation
microbiologique
des
médiastinites
après
chirurgie
cardiaque.
Microbiology
of
mediastinitis
Gram
positive
Cocci
Staphylococcus
aureus
40%
Coagulase
negative
Staphylococcus
30%
Gram
negative
Bacilli
Escherichia
coli
5%
Enterobacter
spp.
10%
Klebsiella
spp.
3%
Proteus
spp.
2%
Pseudomonas
spp.
2%
Other
Candida
<
2%
Polymicrobial
10–40%
From
[29].
6.
Risk
factors
associated
with
mediastinitis
Many
authors,
over
the
last
20
last
years,
have
well
described
the
risk
factors
for
mediastinitis,
especially
in
patients
having
undergone
coronary
bypass,
which
often
overlap.
The
patients
may
be
contaminated
before,
during,
or
after
surgery,
and
any
re-
operation
exposes
to
the
risk
of
SSI.
The
risk
factors
are
related
to
the
patient
(age,
sex,
obesity,
diabetes,
respiratory
insufficiency),
to
surgery
(context
of
emergency,
type
of
surgery,
operative
time,
early
surgical
revision
for
bleeding)
and
to
hospitalization
and
its
environment
(duration
of
preoperative
stay,
patient
preparation)
[8,29,30].
The
main
risk
factors
associated
with
postoperative
SSI
are
listed
in
Table
2.
6.1.
Risk
factors
related
to
patients
Obesity
was
identified
as
an
independent
risk
factor
for
mediastinitis
by
many
authors.
The
severely
obese
patients
Table
2
Main
risk
factors
for
mediastinitis
after
cardiac
surgery.
Principaux
facteurs
de
risque
pour
une
médiastinite
après
chirurgie
cardiaque.
Main
risk
factors
of
mediastinitis
References
Related
to
patients
Age
[31]
Sex
[29,31]
Obesity
[30–32]
Diabetes
[31,33]
COBP
[15,29,31]
Nasal
Staphylococcus
aureus
carriage
[24,34]
Related
to
hospitalization
Duration
of
preoperative
hospitalization
[30]
Related
to
surgery
Surgical
time
[1,33]
Coronary
bypass [15]
Use
of
internal
mammary
arteries
[1,15,35–38]
Early
revision
for
bleeding
[15]
Other
NNIS
infectious
risk
score
≥
2
[15]

Please
cite
this
article
in
press
as:
Lepelletier
D,
et
al.
Epidemiology
and
prevention
of
surgical
site
infections
after
cardiac
surgery.
Med
Mal
Infect
(2013),
http://dx.doi.org/10.1016/j.medmal.2013.07.003
ARTICLE IN PRESS
+Model
MEDMAL-3432;
No.
of
Pages
7
4
D.
Lepelletier
et
al.
/
Médecine
et
maladies
infectieuses
xxx
(2013)
xxx–xxx
[BMI
>
35
kg/m2]
had
increased
risks
for
comorbidity
because
of
a
longer
hospital
stay
than
non-obese
patients,
and
a
lower
5-
year
survival
rate
with
a
Kaplan
Meier
analysis
and
multivariate
analysis
using
Cox’s
regression
model
[32].
The
peri-operative
antibiotic
doses
administrated
to
obese
patients,
not
adapted
to
their
distribution
volume,
and
the
difficulties
to
implement
an
operative
field
could
account
for
this
risk
[39].
Diabetes,
and
especially
peri-operative
hyperglycemia,
also
increases
the
infectious
risk
after
cardiac
surgery.
More
precisely,
elevated
glycemia
(>
200
mg/dL)
on
the
first
and
second
postoperative
days
could
be
associated
to
an
increase
of
sternal
infections
in
diabetic
patients
and
peroperative
control
of
glycemia
could
decrease
the
morbidity
[33].
6.2.
Risk
factors
related
to
the
procedure
Some
surgical
techniques
may
also
be
associated
with
the
risk
of
mediastinitis.
This
is
why
using
either
of
the
two
internal
thoracic
arteries
(ITA)
in
patients
for
coronary
bypass
remains
quite
controversial
[35].
Using
the
two
ITA
results
in
a
signif-
icant
improvement
of
survival
and
of
postoperative
outcome.
Man
authors
have
reported
a
decrease
revision
surgery
rate
for
revascularization
compared
to
patients
whose
bypass
was
made
with
the
great
saphenous
vein.
These
assets
are
counterbalanced
by
the
significantly
increased
risk
of
SSI,
especially
in
obese
and
diabetic
patients
who
should
benefit
the
most
from
the
dou-
ble
internal
thoracic
vascularization
[36].
There
are
alternative
procedures
for
these
patients
including
the
strict
control
of
peri-
operative
glycemia
[37]
and
the
skeletonization
of
arterial
grafts,
minimizing
sternal
devascularization
[38].
The
other
risk
factors
related
to
surgery
are,
early
revision
surgery,
the
more
often
for
postoperative
hemorrhage,
often
mentioned
as
a
risk
factor
for
sternal
infection,
especially
when
the
initial
surgery
was
long
and
complicated
[15,40].
A
mediastinal
hematoma
may
develop,
because
of
the
bad
hemostatic
quality
of
sternal
closure,
favoring
serous
fluid
collection
and
necrotic
material
in
which
bacteria
may
proliferate
[41].
7.
Prevention
strategy
The
occurrence
of
a
postoperative
SSI
is
due
to
several
factors
and
its
prevention
relies
on
the
control
of
risk
factors
related
to
patients,
to
the
procedure,
and
to
hospital
environ-
ment,
during
the
pre,
per,
and
postoperative
periods.
The
French
Society
for
Hospital
Hygiene
(French
acronym
SFHH)
issued
recommendations
for
the
prevention
of
SSI
in
2004,
“Preop-
erative
management
of
the
infectious
risk”
in
partnership
with
all
surgery
learned
societies
[7],
“Air
management
in
the
oper-
ating
room”
[42],
and
more
recently
in
2010
“Monitor
and
prevent
care
related
infections”
in
collaboration
with
the
French
National
Authority
for
Health
(French
acronym
HAS)
[8].
The
2004
recommendations
are
currently
being
reviewed
to
take
into
account
the
evolution
of
published
scientific
data
on
nasal
S.
aureus
decolonization
to
decrease
the
rate
of
S.
aureus
SSI
and
on
the
patient’s
skin
preparation.
The
1999
CDC
recom-
mendations
[10]
in
the
USA
have
been
completed
more
recent
publications,
specifically
adapted
to
cardiac
surgery
[43],
espe-
cially
postoperatively
at
home
[44].
These
measures
are
classified
by
levels
of
recommendations
and
of
evidence
(Table
3).
They
especially
concern
the
preopera-
tive
period
and
include
the
patient’s
body
skin
preparation
(body
hair
removal,
preoperative
shower,
antisepsis
of
the
operative
site
with
an
alcohol
based
antiseptic),
preparation
and
dressing
of
the
surgical
team,
and
environment
control
of
the
operating
room
and
devices.
These
prevention
measures
were
completed
by
recommendations
on
surgical
antibioprophylaxis
issued
by
the
French
Society
of
Anesthesiology
and
Critical
Care
[6]
and
specific
cardiac
surgery
data
[45].
The
decolonization
of
nasal
S.
aureus
carriage
is
currently
the
most
debated
prevention
measure
related
to
the
patient.
Many
authors,
between
2000
and
2010,
reported
no
significant
impact
of
decolonization
on
the
rate
of
S.
aureus
SSI
because
of
differences
in
the
methodological
approach
of
decolonization
strategies
and
types
of
procedures
studied
[24,34].
The
authors
of
a
randomized,
double
blind,
placebo
controlled
study
made
in
2010,
in
the
context
of
a
multicentric
clinical
trial,
reported
the
effectiveness
of
rapid
S.
aureus
screening
on
admission
and
nasal
decolonization
with
mupirocine
only
in
patients
identi-
fied
as
S.
aureus
carriers,
associated
to
body
showering
with
chlorhexidine
gluconate
antiseptic
soap,
and
oro-pharyngeal
decolonization,
on
the
rate
of
deep
S.
aureus
infections,
essen-
tially
in
cardiac
surgery
(the
study
also
included
other
types
of
surgery
but
in
smaller
samples)
compared
to
the
placebo
con-
trol
group
including
patients
carrying
S.
aureus
(79%
decrease,
OR
0.21.
CI95% 0.07–0.62)
[46].
The
trial
results
will
soon
be
integrated
in
the
new
recommendations
of
the
French
Society
for
Hospital
Hygiene,
to
be
issued
in
2013.
Nevertheless,
the
implementation
mode
of
this
decolonization
strategy
(with
or
without:
prior
nasal
screening,
screening
method,
decoloniza-
tion
period)
must
still
be
evaluated
and
the
occurrence
of
SSI
due
to
other
microorganisms
must
be
monitored.
Using
a
sponge
impregnated
with
local
diffusion
antibiotics
on
the
operative
site
(gentamycin)
is
debated
as
a
peroperative
prevention
measure;
recent
scientific
publications
on
this
issue
are
often
contradic-
tory
[47,48].
This
measure
has
not
sufficiently
demonstrated
its
effectiveness,
even
if
some
cardiac
surgery
units
use
it
success-
fully.
The
authors
of
recent
studies
have
reported
the
contribution
of
education
programs
and
of
prevention
focusing
on
some
meas-
ures
grouped
as
“bundles”,
set
of
measures,
which
observed
and
assessed
at
the
same
time,
allow
obtaining
a
decrease
of
SSI
rates,
demonstrating
the
multimodal
aspect
of
prevention
strategies.
These
interventional
programs
include
some
meas-
ures
such
as
the
patient’s
skin
preparation,
nasal
screening
of
patients,
nasal
decolonization
with
mupirocine,
evaluation
and
switch
of
antibioprophylaxis,
especially
for
patients
carrying
methicillin
resistant
S.
aureus
(MRSA),
barrier
measures
in
the
operating
room
(gloves),
and
compression
devices
to
prevent
mechanical
postoperative
scar
disunion
(obese
patients,
patients
presenting
with
chronic
bronchitis),
[49,50].
A
prevention
pro-
gram
implemented
at
the
Nantes
hospital
center
during
more
than
10
years,
allowed
to
decrease
the
rate
of
mediastinitis
100
cardiac
surgery
procedures
from
2.1%
in
2001
to
1.1%
in

Please
cite
this
article
in
press
as:
Lepelletier
D,
et
al.
Epidemiology
and
prevention
of
surgical
site
infections
after
cardiac
surgery.
Med
Mal
Infect
(2013),
http://dx.doi.org/10.1016/j.medmal.2013.07.003
ARTICLE IN PRESS
+Model
MEDMAL-3432;
No.
of
Pages
7
D.
Lepelletier
et
al.
/
Médecine
et
maladies
infectieuses
xxx
(2013)
xxx–xxx
5
Table
3
Prevention
of
surgical
site
infections
(level
and
proof
of
guidelines
2004
and
number
of
recommendation
2010).
Principales
mesures
de
prévention
des
infections
du
site
opératoire
(niveau
de
recommandation
et
de
preuve
2004
et
référence
de
la
recommandation
2010).
Prevention
measures
Recommendations
2004
[7]
Recommendations
2010
[8]
Preoperative
Surveillance
of
surgical
site
infections –
R91
Delayed
surgery
in
case
of
intercurrent
infection
Yes
(A2)
Nasal
Staphylococcus
aureus
decolonization
No
(E-2)a
No
shaving
or
hair
removal
Yes
(B-1)
At
least
one
preoperative
shower
with
antiseptic
soap
Yes
(A-1)aR94
Mouthwash
with
antiseptic
solution
Patient
dressed
with
no-woven
or
micro-fiber
fabric
Yes
(B-1)
Yes
(B-3)
R93
Peroperative
(intra-operating
room)
Disinfection
of
hands
with
hydro-alcoholic
gel
–
Detergence
with
antiseptic
soap
followed
by
broad
disinfection
of
the
operative
site
Yes
(A-1)aR96
Brushing
with
an
alcoholic
antiseptic
solution
Yes
(B-3)aR94
100%
cotton
patient
drapes
No
(E-3)
Adequate
surgical
garb,
operating
room
discipline
and
use
of
a
check-list
–
R97
Quality
of
air
the
operating
room
–
R98
Postoperative
Maintaining
glycemia
<
2
g/L
Yes
(A-1)
Mouthwash
with
antiseptic
solution
Yes
(B-1)
Traceability
of
the
following
Yes
(B-3)
Surgical
program
planning
R97
Antibioprophylaxis
R95
Patient’s
cutaneous
preparation
Identification
of
operators
Elements
of
the
NNIS
infectious
risk
score
Medical
material
and
devices
used
Cleaning
procedures
Chronology
of
events
aUnder
revision
2013.
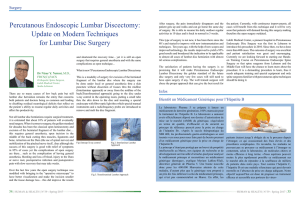
2011
(P
=
0.05)
(Fig.
1).
During
this
period,
the
number
of
pro-
cedures
in
adults
with
extra
corporeal
circulation
increased
from
1100
to
1486,
including
590
coronary
bypass
and
780
valvular
surgery
procedures.
This
prevention
program
chronologically
integrated
several
measures:
retrospective
analysis
of
SSI
and
direct
observation
of
the
patient’s
skin
preparation
(2001),
prospective
surveillance
of
SSI
(2002),
drafting
and
implemen-
tation
of
a
new
operating
mode
for
the
patient’s
skin
preparation
Fig.
1.
Incidence
of
mediastinitis/100
cardiac
surgery
procedures
and
chronology
of
key
prevention
measures
implemented
from
2001
to
2011
at
the
Nantes
university
hospital.
Évolution
du
taux
d’incidence
des
médiastinites/100
interventions
en
chirurgie
cardiaque
et
chronologie
des
principales
mesures
de
prévention
implémentées
sur
une
période
de
11
ans
(2001–2011)
au
centre
hospitalier
universitaires
de
Nantes.
 6
6
 7
7
1
/
7
100%