Saudi J Kidney Dis Transpl 2013;24(4):777-782
© 2013 Saudi Center for Organ Transplantation
Case Report
Profound Nephrotic Syndrome in a Patient with Ovarian Teratoma
Abdallah Jeroudi1, Huseyin Kadikoy1, Lillian Gaber2, Venket Ramanathan1, Adam Frome1,
Nabeel Anwar1, Abdul Abdellatif1
1Baylor College of Medicine and 2The Methodist Hospital, Houston, TX, USA
ABSTRACT. The nephrotic syndrome (NS) has been associated with a variety of malignancies in
a number of reports in the literature, but has been reported in only nine cases associated with
ovarian neoplasms. Membranous nephropathy is the most common glomerular pathology causing
the NS in patients with solid tumors. There has been only one report of an ovarian neoplasm
associated with minimal change disease (MCD). We describe the case of a 36-year-old woman
who presented with the NS secondary to biopsy-proven MCD, likely secondary to mature ovarian
teratoma. Treatment by tumor removal and prednisone led to remission of the NS. To the best of
our knowledge, this is the first report of an ovarian teratoma and the second report of an ovarian
neoplasm associated with MCD.
Introduction
The association between the nephrotic syn-
drome (NS) and a variety of malignancies has
been reported in the literature beginning in
1966.1Among the histologic variants, mem-
branous nephropathy (MN) is the most com-
mon cause of the NS associated with solid tu-
mors,2,3 while minimal change disease (MCD)
has been described in patients with Hodgkin’s
lymphoma (HL).4,5 However, the association
of the NS with ovarian neoplasms is rare and
only nine cases have been reported in the
literature.1,6-12 To the best of our knowledge,
this is the first report of an ovarian teratoma
Correspondence to:
Dr. Abdul Abdellatif,
Assistant Professor of Medicine,
Baylor College of Medicine, 1709 Dryden
Suite 900, Houston, TX 77030, USA
E-mail: Abdula@BCM.EDU
and the second report of an ovarian neoplasm
associated with MCD.12
Case Report
A 36-year-old Hispanic–American woman,
with past medical history significant for pre-
eclampsia two years prior to presentation, was
referred for evaluation of new-onset gene-
ralized edema. The patient was previously
asymptomatic until one week prior to presen-
tation when she developed fatigue, dyspnea on
exertion, foamy urine and generalized edema,
with a 7 lbs weight gain. The patient had labo-
ratory evaluation at an outside facility, which
showed normal kidney function, proteinuria,
hypoalbuminemia and elevated serum choles-
terol, which prompted the referral for eva-
luation and management of the NS.
Her vital signs on initial evaluation were as
follows: Blood pressure 122/87 mmHg, heart
rate 111 beats/min and temperature 36.39°C.
Saudi Journal
of Kidney Diseases
and Transplantation
[Downloaded free from http://www.sjkdt.org on Wednesday, February 26, 2020, IP: 154.121.28.117]

Physical examination was normal except for
bilateral lower extremity edema. Cardiopul-
monary examination was unremarkable. Abdo-
minal examination did not show masses or
hepatosplenomegaly. No generalized lympha-
denopathy was noted. Dipstick urinalysis was
significant for 4+ proteinuria and urine mic-
roscopic examination showed rare red cells.
No cellular casts were seen. Repeat laboratory
tests showed total cholesterol of 317 mg/dL,
total serum protein of 4.2 g/dL, serum albumin
of 1.2 g/dL, blood urea nitrogen of 33 mg/dL
and creatinine of 1.1 mg/dL. Furthermore, the
anti-nuclear antibody, serum protein electro-
phoresis, hepatitis profile and serum comple-
ments were unremarkable.
Ultrasound-guided biopsy of the right kidney
was performed. The needle-core biopsy had
ample renal cortex with at least 22 glomeruli.
The glomeruli were unremarkable by light
microscopy evaluation, with the exception of
minimal and focal increase in mesangial cellu-
larity seen in a few glomeruli (Figure 1).
Lesions of focal and segmental glomeruloscle-
rosis were not noted in multiple-step sections.
Likewise, the tubules exhibited minimal chan-
ges, namely vacuolization of the tubular epi-
thelial cells and a single mitosis without any
obvious changes suggestive of acute tubular
necrosis. There was no interstitial fibrosis. The
blood vessels were normal. Evaluation of the
frozen tissue for immunoglobulins and com-
plement components was negative and there
was no evidence of monoclonal paraprotein
deposition in the tissue. Ultrastructural exami-
nation revealed diffuse effacement of the foot
processes along with features of hypertrophy
and reactive changes in the podocytes (Figure
2). These consisted of hypertrophy of intra-
cytoplasmic organelles and prominent intra-
cellular filaments toward the epi-membranous
portions of the cell body. Electron-dense depo-
sits were not detected. Significant swelling of
the endothelial cells in the glomerular capil-
laries was also noted. Fibrin tactoids was iden-
tified in the lumen of rare glomerular capil-
laries.
After the kidney biopsy, the patient de-
veloped borderline low-blood pressure and her
Figure 1. Normal glomerulus by light micros-
copy. A single mitosis in otherwise normal-
appearing proximal convoluted tubules is seen
(PAS-H-stained section; ×20 original magnifi-
cation).
Figure 2. Electron micrograph of a portion of a
glomerulus showing diffuse effacement of the
foot processes and micro-villous hyperplasia.
The glomerular endothelial cells appear reactive
as they display hypertrophy of the intra-cyto-
plasmic organelles (uranyl acetate and lead
citrate; ×5000).
hemoglobin had dropped from a baseline value
of 14.6 g/dL to 12.9 g/dL, which prompted eva-
luation to rule out possible post-biopsy bleed.
Ultrasound showed a small peri-nephric hema-
778 Jeroudi A, Kadikoy H, Gaber L, Ramanathan V, Frome A, Anwar N, Abdellatif A
[Downloaded free from http://www.sjkdt.org on Wednesday, February 26, 2020, IP: 154.121.28.117]

toma and moderate free fluid in the pelvis.
Computerized tomography scan of the abdo-
men and pelvis was performed to further eva-
luate the pelvic fluid, which revealed a 7 cm
left adnexal mass consistent with ovarian tera-
toma (Figure 3).
The patient underwent laparascopic left
salpingo-oophorectomy and surgical pathology
confirmed a benign mature cystic teratoma.
We contemplated on watchful waiting after
tumor removal for resolution of proteinuria.
She was managed with diuretics, statin and
angiotensin-converting enzyme inhibitor. How-
ever, in view of profound anasarca and signi-
ficant weight gain, she was started on oral
prednisone. She had a brisk response with
resolution of her symptoms and the NS with
less than four weeks of therapy. Her kidney
function improved to baseline serum creatinine
of 0.7 mg/dL.
Discussion
The NS and its association with malignancy
is an uncommon occurrence that was first
documented in the literature by Lee et al in
1966, when he described the presence of the
NS and glomerular pathology in conjunction
with a variety of malignancies. He reported 11
patients without evidence of renal amyloidosis,
renal vein thrombosis or renal involvement of
cancer.1In the absence of an etiology for the
NS occurring around the time of diagnosis of
cancer, he postulated that the body’s response
to tumor products and antigens may be res-
ponsible for the NS and associated glomerular
pathology. In essence, he postulated the occur-
rence of a para-neoplastic syndrome.1
Defined as a clinical disorder that accom-
panies malignancy, para-neoplastic syndromes
are caused by the release of tumor products
and are not directly related to mass effects or
invasion.13,14 Review of the literature by
Bacchetta et al14 documents a large collection
of case reports associating the presence of the
NS as a possible para-neoplastic phenomenon
of a wide array of different neoplasms. To
theoretically qualify as a para-neoplastic syn-
drome, Bachetta et al14 outlines well the gen-
Figure 3. Computerized tomography of the
abdomen and pelvis without intravenous or oral
contrast showing a 7 cm maximal diameter
ovarian teratoma involving the left adenxa. In
the surrounding mesentery, diffuse infiltrative
changes are seen suggesting edema with a small
amount of free pelvic fluid.
eral requirements: (a) Absence of other ob-
vious alternative etiology; (b) temporal rela-
tionship between the NS and cancer diagnosis;
(c) remission of the syndrome clinically and
histologically by either surgery or chemothe-
rapy and (d) worsening of the symptoms with
tumor recurrence. Two limitations in the lite-
rature concerning this definition involve the
ethical implications of verifying histological
remission of the NS by kidney biopsy2 and
inability to completely cure many of the can-
cers reported as associated with this syn-
drome.2,15 Compounding these issues is the
lack of identification of the mechanism leading
to para-neoplastic NS.2,14 Although the mecha-
nism of the para-neoplastic NS is hard to
establish,2,14 a link is suggested by the time
relationship between development of the NS
and detection of cancer as well as several
examples of resolution of proteinuria after
tumor removal7,15-17 and treatment.3,5
Despite limitations in identifying a physical,
mechanistic link between the NS and malig-
nancy, the literature does show an association
between certain glomerular pathological fin-
Profound nephrotic syndrome in ovarian teratoma 779
[Downloaded free from http://www.sjkdt.org on Wednesday, February 26, 2020, IP: 154.121.28.117]

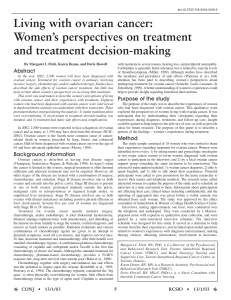
Table 1. Pathological findings and outcomes of cases with ovarian tumor associated with the nephrotic syndrome reported in the literature.
Patient
Age/
gender
Ovarian
malignancy type
Pathological finding
Treatment
Remission of
nephrotic syndrome
Outcome of
cancer
Reference
1
65/Female
Adenocarcinoma
Membranous
nephropathy
None
No
Death
1
2
28/Female
Dermoid cyst
Membranous
nephropathy
Excision,
prednisone
No
Unknown
1
3
65/Female
Papillary serous
carcinoma
Membranous
nephropathy
Excision,
cisplatin,
adriamycin,
cytoxan
Yes
Remission
6
4
Unknown
Carcinoma
Unknown
Unknown
Unknown
Unknown
7
5
7/Female
Benign teratoma
Membranous
nephropathy
Yes
Yes
Remission
8
6
68/Female
Serous
adenocarcinoma
Unknown
Excision,
paclitaxel,
carboplatin
Yes
Death
9
7
15/Female
Mixed germ cell
tumor (embryonal
and dysgerminoma
components)
Membranoproliferative
glomerulonephritis
Excision,
prednisone
No, developed chronic
kidney disease
Unknown
10
8
59/Female
Carcinoma
Membranous
nephropathy
Taxol,
carboplatin,
topotecan,
gemcitabine,
oxaliplatin,
capecitabine
Yes
Remission
11
9
55/Female
Papillary serous
carcinoma
Minimal change
diseases
Excision,
prednisone,
paclitaxel,
carboplatin
Yes
Remission
12
10
36/Female
Benign mature
cystic teratoma
Minimal change
diseases
Excision,
prednisone
Yes
Remission
Present
case
780 Jeroudi A, Kadikoy H, Gaber L, Ramanathan V, Frome A, Anwar N, Abdellatif A
[Downloaded free from http://www.sjkdt.org on Wednesday, February 26, 2020, IP: 154.121.28.117]

dings and certain malignancies.2-5,14 To date,
the NS, in patients with solid tumors, is com-
monly caused by MN,2,3,14 while MCD has
mainly been described in HL,4,5,14 and other
hematological malignancies.14 While MCD has
been observed in cases of the NS associated
with solid tumors, the review by Bacchetta et
al14 in 2009 highlights this uncommon finding
by reporting only 64 cases in the literature.
In terms of ovarian malignancies associated
with the NS, case reports are rare, with only
nine other cases reported in the literature.1,6-12
In all but two of these cases, the glomerular
pathology was known (Table 1). Pathological
diagnoses reveal that five of the seven biopsy-
proven cases were associated with MN,1,6,8,11
which is in line with the concept that solid
tumors associated with the NS tend to display
MN on pathological examination.2,3,14 One of
the seven biopsy-proven cases showed mem-
branoproliferative glomerulonephritis on histo-
logy.10 To the best of our knowledge, this is
the first report of ovarian teratoma associated
with MCD and the second case of ovarian
neoplasm to be associated with MCD.12
Remission of the NS should theoretically
accompany tumor removal and treatment of
the culprit disease process, but that is not al-
ways the case in the literature.14 Cases detai-
ling the resolution of the NS rapidly after
tumor removal without adjunct treatments are
extremely rare,8,16,17 but theoretically provide
the strongest link between the NS and cancer.14
Other cases involving the use of steroids and
immuno-suppressants for cancer treatment
may pose a dilemma as these compounds are
also used to treat MCD and MN.18 Con-
versely, it can be argued that successful treat-
ment of the cancer causes remission of the NS.
In the retrospective study of 21 patients with
MCD-related NS and HL by Audard et al,5
patients in a sub-group of the NS, poorly res-
ponsive to steroids, achieved remission of the
NS with successful treatment of HL by chemo-
therapy.
In the case reports of ovarian malignancies
associated with the NS, the results are mixed
concerning remission of the NS and ovarian
cancer (Table 1). Remission of the NS was
seen in five cases that achieved successful
treatment of ovarian cancer: One by excision
alone;8 one by chemotherapy alone;11 and three
by excision with chemotherapy.6,9,12 On the
other hand, remission of the NS was not
achieved in a patient with mixed-germ cell
ovarian tumor treated with prednisone and
excision;10 yet, this could have been secondary
to the development of chronic kidney disease.
In the two cases reported by Lee et al,1 remis-
sion of the NS was not seen in the patient who
died without receiving treatment as well as the
patient who had received prednisone and exci-
sion of the ovarian dermoid cyst. Treatment
and outcome could not be analyzed in one of
the cases due to incomplete information.7
Several factors in this case strengthen the
association of MCD and the ovarian teratoma.
First, MCD NS is classically a childhood con-
dition,18 and accounts for only 10–15% of
adult cases, 18,19 with an average age at onset of
45.1 years and a standard deviation of 1.6
years.20 Second, there is an excellent temporal
relationship between diagnosis of cancer and
onset of symptoms. The patient lacked any
significant medical history considered to be
associated with secondary MCD picture such
as drugs, infection, atopy and certain chronic
medical conditions.21 Third, even though the
remission rate is excellent in adult patients
with MCD, the time to response is prolonged.
Our patient responded very briskly to surgical
removal of tumor and short-term prednisone
therapy. Despite limitations in identifying a
physical, mechanistic link between MCD and
ovarian teratoma, future reports and studies
may lead to such findings.
References
1. Lee JC, Yamauchi H, Hopper J Jr. The asso-
ciation of cancer and the nephrotic syndrome.
Ann Intern Med 1966;64:41-51.
2. Ronco PM. Paraneoplastic glomerulopathies:
New insights into an old entity. Kidney Int
1999;56:355-77.
3. Lefaucheur C, Stengel B, Nochy D, et al.
Membranous nephropathy and cancer: Epide-
miologic evidence and determinants of high-
risk cancer association. Kidney Int 2006;70:
Profound nephrotic syndrome in ovarian teratoma 781
[Downloaded free from http://www.sjkdt.org on Wednesday, February 26, 2020, IP: 154.121.28.117]
 6
6
1
/
6
100%