Fecal incontinence
DRE SUSANNA SCARSI
04.07.2019
Dre Celine Duvoisin

Epidemiology
- Very common
-Under-reported
-True prevalence difficult to assess
-Reported prevalence 0.4%-18%
-F:M 63%:37%
-30% older than 65 years
Bharucha et al - Am J Gastroenterol. -2015
Ditah et al - Clin Gastroenterol Hepatol. - 2014

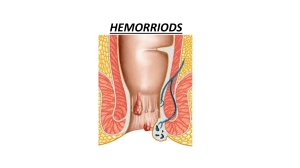
Definition
•Involuntary loss of rectal contents (feces, gas) through the anal canal and the
inability to postpone an evacuation until socially convenient.
•Fecal incontinence classified as:
opassive incontinence (involuntary discharge without any awareness)
ourge incontinence (discharge despite active attempts to retain contents)
ofecal seepage (leakage of stool with grossly normal continence and evacuation)
Ruiz and Kaiser - World J Gastroenterol -2017

Etiology
Rao et al - Am J Gastroenterol. - 2004

Risk factors
•Older age
•Diarrhea
•Fecal urgency
•Urinary incontinence
•Diabetes mellitus
•Hormone therapy
Bharucha et al - Am J Gastroenterol. -2015
 6
6
 7
7
 8
8
 9
9
 10
10
 11
11
 12
12
 13
13
 14
14
 15
15
 16
16
 17
17
 18
18
 19
19
 20
20
 21
21
 22
22
 23
23
 24
24
 25
25
 26
26
 27
27
 28
28
 29
29
 30
30
 31
31
 32
32
 33
33
 34
34
 35
35
1
/
35
100%