ClC-3 expression enhances etoposide resistance by increasing acidification of the late

ClC-3 expression enhances etoposide resistance by
increasing acidification of the late
endocytic compartment
Karsten H. Weylandt,
1
Maxim Nebrig,
1,2
Nils Jansen-Rosseck,
1,2
Joanna S. Amey,
2
David Carmena,
2
Bertram Wiedenmann,
1
Christopher F. Higgins,
2
and Alessandro Sardini
2
1
Department of Gastroenterology, Charite´ University Medicine,
Campus Virchow-Klinikum, Berlin, Germany and
2
Medical
Research Council Clinical Sciences Centre, Imperial College
Faculty of Medicine, Hammersmith Hospital Campus, London,
United Kingdom
Abstract
Resistance to anticancer drugs and consequent failure of
chemotherapy is a complex problem severely limiting
therapeutic options in metastatic cancer. Many studies
have shown a role for drug efflux pumps of the ATP-
binding cassette transporters family in the development of
drug resistance. ClC-3, a member of the CLC family of
chloride channels and transporters, is expressed in
intracellular compartments of neuronal cells and involved
in vesicular acidification. It has previously been suggested
that acidification of intracellular organelles can promote
drug resistance by increasing drug sequestration. There-
fore, we hypothesized a role for ClC-3 in drug resistance.
Here, we show that ClC-3 is expressed in neuroendocrine
tumor cell lines, such as BON, LCC-18, and QGP-1, and
localized in intracellular vesicles colabeled with the late
endosomal/lysosomal marker LAMP-1. ClC-3 overexpres-
sion increased the acidity of intracellular vesicles, as
assessed by acridine orange staining, and enhanced
resistance to the chemotherapeutic drug etoposide by
almost doubling the IC
50
in either BON or HEK293 cell
lines. Prevention of organellar acidification, by inhibition of
the vacuolar H
+
-ATPase, reduced etoposide resistance.
No expression of common multidrug resistance trans-
porters, such as P-glycoprotein or multidrug-related pro-
tein-1, was detected in either the BON parental cell line or
the derivative clone overexpressing ClC-3. The probable
mechanism of enhanced etoposide resistance can be
attributed to the increase of vesicular acidification as
consequence of ClC-3 overexpression. This study there-
fore provides first evidence for a role of intracellular CLC
proteins in the modulation of cancer drug resistance. [Mol
Cancer Ther 2007;6(3):979 –86]
Introduction
Metastatic cancers are usually treated using chemotherapy
regimens to target tumor cells disseminated throughout the
organism. Yet, although the initial response to treatment
might be good, multidrug resistance eventually emerges,
leading to treatment failure and death. Several mechanisms
are responsible for the development of drug resistance at a
cellular level. Although it has been shown that target
modification can lead to drug resistance, it is frequently the
emergence of expression of ATP-binding cassette trans-
porters, responsible for drug efflux from cancer cells, that
actually leads to resistance (1). Proteins of this family have
also been shown to sequester drugs in intracellular
membrane compartments, thereby decreasing effective
drug concentrations and inducing resistance (2).
Intracellular acidic compartments can sequester basic
anticancer drugs, which accumulate passively in response
to the pH gradient, and thus contribute to drug resistance.
Several studies have implied a link between drug resistance
and intravesicular acidity either by comparison of drug-
sensitive and drug-resistant cell lines (3, 4) or through
treatment with agents disrupting organellar pH (5). A
recent study showed that omeprazole, a proton pump
inhibitor used in antiacid treatment of peptic disease, and
the vacuolar proton pump (v-H
+
-ATPase) inhibitor bafilo-
mycin A increased cytotoxicity of the basic chemothera-
peutic drugs doxorubicin and mitoxantrone (6). Similarly,
in vivo studies of human melanoma xenografts in severe
combined immunodeficient mice showed that proton
pump inhibitors affected sensitivity to cisplatin (7).
Moreover, a study with a novel v-H
+
-ATPase inhibitor
showed an increased effectiveness of topotecan chemother-
apy when combined with this inhibitor, supporting the
hypothesis of a role for intracellular acidic compartments in
mediating chemotherapy resistance (8). Vesicular proton
pump inhibition might therefore be a future target option
for increasing the effectiveness of cancer chemotherapy.
Although these studies have focused on the role of
intracellular proton pumps and transporters for chemo-
therapy resistance, the presence also of an anion shunt
current is a requisite for the accumulation of protons in
intracellular membrane compartments. This current is
necessary to dissipate the charge gradient generated by
Received 8/8/06; revised 11/15/06; accepted 1/11/07.
The costs of publication of this article were defrayed in part by the
payment of page charges. This article must therefore be hereby marked
advertisement in accordance with 18 U.S.C. Section 1734 solely to
indicate this fact.
Note: K.H. Weylandt and M. Nebrig contributed equally to this work.
Requests for reprints: Alessandro Sardini, Medical Research Council
Clinical Sciences Centre, Imperial College Faculty of Medicine,
Hammersmith Hospital Campus, Du Cane Road, London W12 0NN,
United Kingdom. Phone: 44-20-8383-8270; Fax: 44-20-8383-8337.
E-mail: [email protected]
Copyright C2007 American Association for Cancer Research.
doi:10.1158/1535-7163.MCT-06-0475
979
Mol Cancer Ther 2007;6(3). March 2007
on July 8, 2017. © 2007 American Association for Cancer Research. mct.aacrjournals.org Downloaded from

the electrogenic activity of the v-H
+
-ATPase during the H
+
transport. Chloride channels/transporters of the CLC
family have been suggested to provide the anion shunt
current (9). We therefore tested the hypothesis of an
involvement of intracellular CLC channels/transporters in
drug resistance.
ClC-3, a member of the CLC family of chloride channels
and transporters, is expressed predominantly in the cells
of the nervous system and is located in acidic intracellular
compartments (10, 11). ClC-3 has been suggested to
generate a shunt current of chloride for v-H
+
-ATPases,
thereby aiding the acidification of endosomes and synaptic
vesicles (10) as well as lysosomes (12). This hypothesis was
confirmed in experiments directly showing a role for ClC-
3 in endosomal acidification (13). The homologous CLC
proteins ClC-5 and ClC-7 play also a role in modulating
the pH of intracellular compartments and vesicle traffick-
ing in the cell (9, 14). Because ClC-3 is expressed in
pheochromocytoma cells (15), we hypothesized the pres-
ence of ClC-3 also in gastrointestinal neuroendocrine
tumor cells.
Etoposide, in combination with a platin substance, is the
mainstay of chemotherapy treatment of undifferentiated,
high-grade neuroendocrine tumors (16 –19) and small cell
lung cancers (20). At the time of diagnosis, these tumors are
mostly disseminated so that systemic chemotherapy
remains as the only applicable treatment option. Although
initial responses to chemotherapy treatment are usually
good with significant reduction of tumor size, most of these
tumors rapidly develop chemotherapy resistance. As a
consequence, nearly all patients with these cancers even-
tually succumb to progressive disease.
As for most other anticancer drugs, etoposide has a basic
pKa (9.8; ref. 21), predisposing it to trapping in acidic
compartments. We therefore investigated the hypothesis
that expression of ClC-3 in a neuroendocrine tumor cell line
increases the acidity of intracellular compartments and
thereby etoposide drug resistance.
Materials and Methods
Cell Culture and Generation of Clonal Cell Lines
BON is a neuroendocrine cell line established from a
human pancreatic neuroendocrine carcinoma (22, 23).
BON cells were cultured at 37jC in a 5% CO
2
and
water-saturated atmosphere and grown in DMEM and
F12 (1:1), 25 mmol/L HEPES, 10% fetal bovine serum
(FBS), and 10 Ag/mL ciprofloxacin (Ciprobay). LCC-18 is a
cell line established from a human neuroendocrine-
differentiated colonic carcinoma (24). LCC-18 cells were
cultured in RPMI 1640, 10% FBS, insulin, transferrin, and
selenium liquid medium supplement (Sigma, St. Louis,
MO), and 10 Ag/mL ciprofloxacin (Ciprobay). QGP-1 cells,
a human pancreatic carcinoma cell line of islet origin
(25), were cultured in DMEM and 10% FBS. PC12 cells are
an established line derivative of a rat pheochromocytoma
and were cultured in high-glucose DMEM, 10% FBS,
and 5% horse serum. CaCo-2 is a cell line established
from an adenocarcinoma of the colon and was cultured in
MEM plus 10% FCS. The BON cell clone permanently
overexpressing ClC-3-green fluorescent protein (GFP)
was generated by transfection with the pCIneo plasmid
coding for the fusion protein and selection in G418
following a similar procedure used to generate the
HEK293 clone expressing ClC-3-GFP (11). HEK293 clone
expressing ClC-3-GFP was cultured in DMEM, 10% FBS,
and 500 Ag/mL G418. NIH3T3-MDR1 cell line (26), a
derivative of the mouse fibroblast NIH3T3 line, perma-
nently transfected with the human MDR1 gene coding
for P-glycoprotein, was grown in DMEM, 10% FBS, and
1Ag/mL colchicine. SW-620 cell line, derived from a
human colon adenocarcinoma (27), was grown in RPMI
1640 and 10% FBS.
Total Membrane Preparation and Western Blotting
Cells, cultured as described above, were homogenized
and crude membrane preparation was obtained (see
Supplementary Data for a detailed description).
3
Membrane
proteins were resolved by SDS-PAGE and transferred onto
polyvinylidene difluoride membranes (Immobilon-P, Milli-
pore, Billiberia, MA). ClC-3 proteins were detected with the
D1-specific polyclonal antibody against ClC-3 (1:100 over-
night at 5jC; ref. 11), P-glycoprotein was detected with the
monoclonal antibody C219 (1:1,000 overnight; Dako, Car-
pinteria, CA), and the multidrug-related protein-1 (MRP-1)
was detected with the monoclonal antibody MRPm5 (1:50
overnight; Abcam, Cambridge, United Kingdom) followed
by appropriate horseradish peroxidase secondary anti-
bodies (1:1,000; Dako). Signal was visualized by chemilu-
minescence (Amersham ECL system; Amersham, Little
Chalfont, United Kingdom). A detailed description of
the Western blotting procedure is available in the Supple-
mentary Data.
3
Immunocytochemistry, Life Stains, and Confocal
Imaging
For immunocytochemistry on BON cells permanently
transfected with ClC-3-GFP, cells were plated on poly-L-
lysine–coated (Sigma) glass coverslips and cultured in six-
well plates for 24 to 48 h before fixation with a solution of
4% formaldehyde/4% sucrose in PBS buffer or methanol at
20jC. Cells were then permeabilized with 0.1% Triton
X-100 for 4 min and costained with antibodies against
chromogranin A (DAK-A3; Dako), synaptophysin (gift from
C. Groetzinger, Charite´ University Medicine, Campus
Virchow-Klinikum, Berlin, Germany), EEA-1 (1:50; Santa
Cruz Biotechnology, Santa Cruz, CA), and LAMP-1 (1:50;
Santa Cruz Biotechnology) for 12 h at 4jC after blocking
with 0.2% fish skin gelatin in PBS. All primary antibodies
were detected by appropriate secondary antibody conju-
gated to the fluorophore Alexa Fluor 568 (1:600; Molecular
Probes/Invitrogen, Carlsbad, CA). Cells were also stained
with 4¶,6-diamidino-2-phenylindole (DAPI; 15 mg/mL;
1:10,000 dilution; Molecular Probes) for nuclear DNA.
3
Supplementary material for this article are available at Molecular Cancer
Therapeutics Online (http://mct.aacrjournals.org/).
ClC-3 and Cancer Drug Resistance980
MolCancerTher2007;6(3).March2007
on July 8, 2017. © 2007 American Association for Cancer Research. mct.aacrjournals.org Downloaded from

Coverslips were mounted in Vectashield (Vector Laborato-
ries, Burlingame, CA) for examination and cells were
imaged using a Leica SP confocal microscope equipped
with a 100/1.4 NA PlanApoChromat oil immersion
objective lens (Leica, Wetzlar, Germany) as described in
the Supplementary Data.
3
Analysis of LAMP-1 signal at the
fluorescence-activated cell sorting was conducted by fixing
the resuspended cells in 70% ice-cold methanol and staining
for LAMP-1 with the above described antibody (1:50) for
2 h at room temperature in 0.2% fish skin gelatin, and then,
the primary antibody was recognized by goat anti-mouse
Cy5-conjugated antibody (1:200; 30 min at room tempera-
ture; Abcam; see Supplementary Data for details of
fluorescence-activated cell sorting settings).
3
Control was
obtained by exposure of the preparation to the secondary
antibody only. To identify acidic compartments, live BON
cells expressing ClC-3-GFP were stained for 30 min at 37jC
with 50 nmol/L DND-99/LysoTracker Red, a low pH-
specific fluorophore (Molecular Probes). Cells were imaged
in a perfusion chamber with a Leica SP confocal microscope
equipped with 631.32 NA PlanApoChromat oil immer-
sion objective, and to avoid bleed through, the fluorophores
were excited sequentially as described in the Supplemen-
tary Data.
3
Similarly, identification of acidic compartments
was achieved by staining the cells in the perfusion chamber
for 5 min with 10 Amol/L acridine orange (Molecular
Probes) until organelle steady-state accumulation was
reached (see Supplementary Data and the next paragraph
for further details).
3
All images were analyzed with Meta-
Morph 5.0v1 software (Universal Imaging, Downingtown,
PA). Figures were assembled for publication with Adobe
Photoshop 6.0 software (Adobe Systems, San Jose, CA).
Quantification of Acridine Orange Fluorescence from
Acidic Compartments
Acridine orange (AO) was used to measure acidic
compartments. The fluorophore accumulates in acidic
compartments of cells where it remains trapped following
protonation. On increasing concentrations of AO, the
spontaneous formation of dimeric AO molecules leads to
a shift in its fluorescence emission maximum from green to
far red, thereby labeling acidic compartments in red (28).
Accumulation in the acidic compartment is dependent on
extracellular acridine orange concentration [AO]
ext
and
proportional to the magnitude of the DpH across the
compartment membrane. When the external pH is kept
constant, the [AO]
int
of the acidic compartment is linearly
proportional to the [AO]
ext
. This was exploited to quantify
the acidic compartment in large numbers of cells by using
flow cytometry (see Supplementary Data
3
and ref. 29 for
further details). Data so acquired were analyzed off-line by
FlowJo (TriStar, Inc., San Carlos, CA). In brief, the mean
average intensity fluorescence signal in the FL-3 channel
from a sample population of 10,000 cells was assessed for
each [AO]
ext
to which cells were exposed. The mean FL-3
intensity values were plotted against the [AO]
ext
and fitted
with a linear regression of the first order by using the
Marquardt-Levenberg algorithm based on the least-square
method (SigmaPlot version 8). The slopes of the relation-
ship obtained for different treatments were statistically
compared by the parallelism test (F test; significantly
different for PV0.05). For each treatment, at least three
independent measurements were done.
Cell Proliferation Assay
Drug cytotoxicity was assessed with the Cell Proliferation
Kit II as described by the manufacturer (Roche Diagnostics,
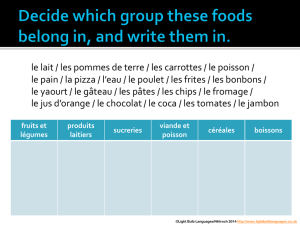
Figure 1. Expression and localization of ClC-3 in neuroendocrine cell
lines. A, Western blot analysis of ClC-3 expression in cell membrane
preparations. Lane 1, PC12 cells; lane 2, BON cell line; lane 3, LCC-18 cell
line; lane 4, CaCo-2 cell line; lane 5, QGP-1 cell line. In each lane, 50 Ag of
total protein were loaded. Molecular weights are in kDa. B, confocal
images of BON cells overexpressing ClC-3-GFP. i, GFP fluorescence in
green;ii, staining of the same cells with LAMP-1 in red ;iii, overlay of (i)
and (ii) with colocalization in yellow. Nuclei are labeled in blue by DAPI
staining. Bar, 10 Am.
Molecular Cancer Therapeutics 981
Mol Cancer Ther 2007;6(3). March 2007
on July 8, 2017. © 2007 American Association for Cancer Research. mct.aacrjournals.org Downloaded from

Indianapolis, IN). Cells were seeded in 96-well tissue
culture plates with 100 AL of appropriate tissue culture
medium. After 24 h, culture medium was exchanged with
fresh medium without phenol red (to avoid interference
with the absorption readings) and containing appropriate
concentration of etoposide (stock solution in DMSO).
Percentage of cell survival was expressed as normalized
average absorption values from four replicates per each
drug concentration FSD. The concentration of drug
required to decrease cell proliferation by 50% (IC
50
) was
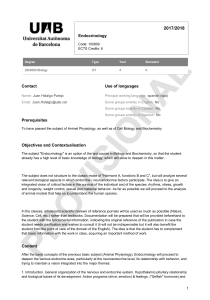
Figure 2. ClC-3 localizes in an acidic compartment of BON cells, increases its acidity, and enhances resistance to etoposide. A, confocal images of live
BON cells overexpressing ClC-3-GFP (green, left) before staining acidic compartments for 5 min with 10 Amol/L acridine orange (red, middle ). Right,
yellow, colocalization of GFP and acridine orange. Blue, nuclei were labeled with DAPI at the end of the experiment following permeabilization. Bar, 10 Am.
B, confocal images of live BON cells overexpressing ClC-3-GFP (green, left ) after 30 min of incubation with 50 nmol/L LysoTracker Red (red, middle ).
Right, yellow, colocalization overlay of GFP and LysoTracker. Bar, 10 Am. C, assessment of acidity of intracellular compartments by flow cytometry
showing mean acridine orange fluorescence intensity of BON cells sorted for high (red trace ) and low (black trace) expression of ClC-3-GFP. The slopes
are significantly different (P< 0.01, F test). D, cell survival after 48 h of exposure to etoposide. BON cells were sorted for high (red trace )orlow(black
trace) expression of ClC-3-GFP. The IC
50
of the two tested cell populations are significantly different (P< 0.01, Student’s ttest); points, data average;
bars, SD.
ClC-3 and Cancer Drug Resistance982
MolCancerTher2007;6(3).March2007
on July 8, 2017. © 2007 American Association for Cancer Research. mct.aacrjournals.org Downloaded from

determined for each treatment from the concentration-
response curve of the 2,3-bis[2-methoxy-4-nitro-5-sulfo-
phenyl]-2H-tetrazolium-5-carboxanilide inner salt assay
and statistically compared by Student’s ttest. The concen-
tration-response curves were obtained by fitting the
experimental data by nonlinear regression with a logistic
curve (SigmaPlot version 8.0).
Results
Western blot analysis (Fig. 1A), using a polyclonal antibody
specific against ClC-3 (11), showed endogenous expression
of ClC-3 in the BON cell line derived from a human
pancreatic neuroendocrine tumor and well established as
a model for neuroendocrine cells (23). ClC-3 was also
expressed in other human neuroendocrine cell lines
derived from tumors of the gastrointestinal tract, such as
LCC-18 and QGP-1. ClC-3 expression was confirmed in
PC12 cells, a cell line derived from rat pheochromocytoma
and previously shown to express ClC-3 (15). In contrast, the
gastrointestinal tumor cell line CaCo-2, established from a
human colon adenocarcinoma, showed significantly lower
levels of ClC-3 expression.
To study the intracellular localization of ClC-3 in
neuroendocrine cells, a clone of BON cells constitutively
expressing a C-terminally GFP-tagged ClC-3 protein was
generated (see Materials and Methods). ClC-3-GFP was
primarily expressed in intracellular vesicles colabeled by
the late endosomal/lysosomal marker LAMP-1 (Fig. 1B).
No colocalization of ClC-3 was observed with markers of
neuroendocrine secretory vesicles, such as chromogranin A
or synaptophysin (data not shown). The late endosomal/
lysosomal compartments are acidic and play a critical role
in cellular metabolism as the site of protein degradation
and of specialized autolytic processes. A v-type H
+
-ATPase
in the vesicular membrane is responsible for establishment
of the acidic intracellular pH. Because this protein is an
electrogenic pump, it is generally assumed that efficient
acidification also requires an anionic shunt current to
abolish the charge buildup generated by the transport of H
+
(9). Live BON cells expressing ClC-3-GFP were stained for
intracellular acidic compartments using either the weak
amine base acridine orange (Fig. 2A) or the red fluorescent
cyanine dye DND-99/LysoTracker Red (Fig. 2B). The
colocalization with fluorescent ClC-3-GFP showed that
ClC-3 resides in the membrane of acidic vesicles.
To assess the acidity of vesicles overexpressing ClC-3, we
used a titration approach using acridine orange as a
fluorophore and flow cytometry analysis (ref. 29; see also
Materials and Methods and Supplementary Data).
3
Briefly,
changes in acidity of intracellular organelles can be
followed by measuring the change in slope of the
relationship between the intensity of AO fluorescence
emission in the far red (FL-3 channel) and the concentration
of [AO]
ext
to which the cells are exposed. To maintain ClC-3-
GFP expression, cells were grown in selective medium
containing G418. This has the drawback that any detectable
functional difference between the overexpressing clone and
the parental cell line could be either associated to the
expression of ClC-3 or to unavoidable and unpredictable
changes due to the selection process. To avoid this, we
exploited the naturally occurring difference in ClC-3-GFP
level expression within cells of the same clone. Clonal BON
cells expressing ClC-3-GFP were fluorescence-sorted for
populations with high and low ClC-3-GFP expression and
compared for acidity of intracellular organelles. Higher
ClC-3-GFP expression conferred an increase of the acidity of
intracellular organelles as shown by a significantly steeper
slope, in comparison with BON cells expressing low ClC-3-
GFP (Fig. 2C). Previous studies have suggested that
intracellular acidic compartments may sequester basic
drugs, thereby decreasing effective concentrations of drug
in the cell nucleus and cytoplasm and, consequently,
cytotoxicity. BON cells sorted for high ClC-3-GFP expres-
sion showed, in comparison with BON cells sorted for low
ClC-3-GFP expression, a significantly increased resistance
to etoposide, a chemotherapeutic drug with a basic pKa
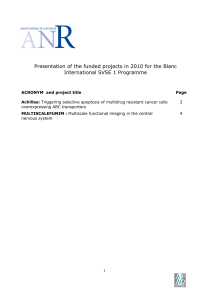
Figure 3. Expression of ClC-3 in HEK293 cells increases the acidity of
intracellular compartment and enhances resistance to etoposide.
A, assessment of acidity of intracellular compartments by flow cytometry
showing mean acridine orange fluorescence intensity of HEK293 cells
sorted for high (red trace) and low (black trace ) expression of ClC-3-GFP.
Slopes are significantly different (P< 0.01, F test). B, cell survival after
48 h of exposure to etoposide. HEK293 cells were sorted for high (red
trace) and low (black trace ) expression of ClC-3-GFP. The IC
50
of the two
tested cell populations are significantly different (P< 0.01, Student’s
ttest); points, data average; bars, SD.
Molecular Cancer Therapeutics 983
Mol Cancer Ther 2007;6(3). March 2007
on July 8, 2017. © 2007 American Association for Cancer Research. mct.aacrjournals.org Downloaded from
 6
6
 7
7
 8
8
 9
9
1
/
9
100%