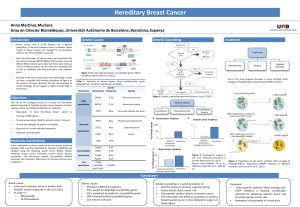
Inherited breast cancer

13.40-14.00 Inherited breast cancer
14.00-14.20 Inherited colon cancer
14.20-14.40 Other inherited cancer predispositions
!" #$$%&!%&'%%$%"
(%$)"%&*%&+,$,)-./% 0/12-$%

(3-$-./%4& /$-5%"4-)2-"%4& 62-$)7'/8&9 #$$%&!%&'%%$%"
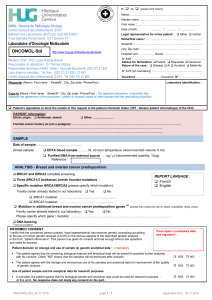
1. INHERITED BREAST CANCER
Introduction
Breast cancer :
clinicopathological features
hormone receptor level (ER and PgR)
HER2
histological grade (1 to 3)
proliferation index (e.g. Ki67)
size (≤2cm, 2.1-5cm, >5cm)
peritumoral vascular invasion
axillary lymph node involvement
#$$&:$8;3<&=>>?&#/@A=>BCDEFGF?7=?
=2

(3-$-./%4& /$-5%"4-)2-"%4& 62-$)7'/8&9 #$$%&!%&'%%$%"
Introduction
Breast cancer : multidisciplinary team
surgeon / gynaecologist
medical oncologist
radiation oncologist
radiologist
pathologist
geneticist
G3

(3-$-./%4& /$-5%"4-)2-"%4& 62-$)7'/8&9 #$$%&!%&'%%$%"
Breast cancer: risk factors
Sex
H1 M / 100 F
Age
Hthe risk increases with age
Hbut 15-20% before the age of 50
Family history
Personal history
Environmental factors (geographic migration)
Prolonged exposure to oestrogens:
HEarly menarche
HLate menopause
HLate first pregnancy, few pregnancies
HLack of breast-feeding
Other breast lesions (in situ carcinoma, atypical hyperplasia, radial scar, ...)
Controversies: endocrine treatment for menopausal status, weight, alcohol,
tobacco, …
I

(3-$-./%4& /$-5%"4-)2-"%4& 62-$)7'/8&9 #$$%&!%&'%%$%"
Introduction
Breast cancer –genetic risk
15% of healthy women have at least one 1st degree relative with breast cancer
!risk x 2
Breast cancer risk increases with the number of 1st degree relatives with breast cancer
1: x 1.8
2: x 2.9
3: x 3.9
BRCA1 and BRCA2 germline mutations are responsible for 20-40% of familial breast
cancer cases, but < 5% of all breast cancers
> 50% of the genetic predisposition to familial breast cancer remains unexplained
J5
Familial cases
Hereditary syndrome
 6
6
 7
7
 8
8
 9
9
 10
10
 11
11
 12
12
 13
13
 14
14
 15
15
 16
16
 17
17
 18
18
 19
19
 20
20
 21
21
 22
22
 23
23
 24
24
 25
25
 26
26
 27
27
 28
28
 29
29
 30
30
 31
31
 32
32
 33
33
 34
34
 35
35
 36
36
 37
37
 38
38
 39
39
 40
40
 41
41
 42
42
 43
43
 44
44
 45
45
1
/
45
100%
![Poster LIBER san antonio 2011 [Mode de compatibilité]](http://s1.studylibfr.com/store/data/000441925_1-0f624c1012097e18f69fca01a2951eb6-300x300.png)